Yonsei Med J.
2014 Jan;55(1):113-117. 10.3349/ymj.2014.55.1.113.
Positive Maternal C-Reactive Protein Predicts Neonatal Sepsis
- Affiliations
-
- 1Department of Pediatrics, CHA Gangnam Medical Center, CHA University, Seoul, Korea.
- 2Department of Pediatrics, Yonsei University College of Medicine, Seoul, Korea. ranng@yuhs.ac
- KMID: 1779894
- DOI: http://doi.org/10.3349/ymj.2014.55.1.113
Abstract
- PURPOSE
To evaluate the diagnostic performance of maternal inflammatory marker: C-reactive protein (CRP) in predicting early onset neonatal sepsis (that occurring within 72 hours after birth).
MATERIALS AND METHODS
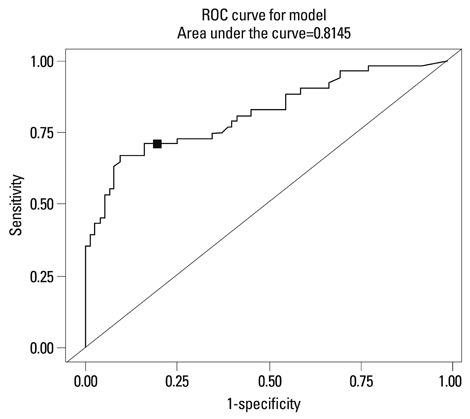
126 low birth weight newborns (gestation 32+/-3.2 wk, birth weight 1887+/-623 g) and their mothers were included. Neonates were divided into sepsis group (n=51) including both proven (positive blood culture) and suspected (negative blood culture but with more than 3 abnormal clinical signs), and controls (n=75). Mothers were subgrouped into CRP positive > or =1.22 mg/dL (n=48) and CRP negative <1.22 mg/dL (n=78) group, determined by Receiver Operating Characteristic curves, and odds ratio was calculated for neonatal sepsis according to maternal condition.
RESULTS
Maternal CRP was significantly higher in neonatal sepsis group than in control (3.55+/-2.69 vs. 0.48+/-0.31 mg/dL, p=0.0001). Maternal CRP (cutoff value >1.22 mg/dL) had sensitivity 71% and specificity 84% for predicting neonatal sepsis. Maternal CRP positive group had more neonatal sepsis than CRP negative group (71% vs. 29%, p<0.001). Odds ratio of neonatal sepsis in maternal CRP positive group versus CRP negative group was 10.68 (95% confidence interval: 4.313-26.428, p<0.001).
CONCLUSION
The risk of early onset neonatal sepsis significantly increased in the case of positive maternal CRP (> or =1.22 mg/dL). In newborn of CRP positive mother, the clinician may be alerted to earlier evaluation for possible neonatal infection prior to development of sepsis.
MeSH Terms
Figure
Reference
-
1. Schuchat A, Zywicki SS, Dinsmoor MJ, Mercer B, Romaguera J, O'Sullivan MJ, et al. Risk factors and opportunities for prevention of early-onset neonatal sepsis: a multicenter case-control study. Pediatrics. 2000; 105(1 Pt 1):21–26.
Article2. Martius JA, Roos T, Gora B, Oehler MK, Schrod L, Papadopoulos T, et al. Risk factors associated with early-onset sepsis in premature infants. Eur J Obstet Gynecol Reprod Biol. 1999; 85:151–158.
Article3. Seaward PG, Hannah ME, Myhr TL, Farine D, Ohlsson A, Wang EE, et al. International multicenter term PROM study: evaluation of predictors of neonatal infection in infants born to patients with premature rupture of membranes at term. Premature Rupture of the Membranes. Am J Obstet Gynecol. 1998; 179(3 Pt 1):635–639.
Article4. Romero R, Gotsch F, Pineles B, Kusanovic JP. Inflammation in pregnancy: its roles in reproductive physiology, obstetrical complications, and fetal injury. Nutr Rev. 2007; 65(12 Pt 2):S194–S202.
Article5. Goldenberg RL, Hauth JC, Andrews WW. Intrauterine infection and preterm delivery. N Engl J Med. 2000; 342:1500–1507.
Article6. Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008; 371:75–84.
Article7. Yoon BH, Yang SH, Jun JK, Park KH, Kim CJ, Romero R. Maternal blood C-reactive protein, white blood cell count, and temperature in preterm labor: a comparison with amniotic fluid white blood cell count. Obstet Gynecol. 1996; 87:231–237.
Article8. Asrat T. Intra-amniotic infection in patients with preterm prelabor rupture of membranes. Pathophysiology, detection, and management. Clin Perinatol. 2001; 28:735–751.
Article9. Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA, et al. Changes in pathogens causing early-onset sepsis in very-low-birth-weight infants. N Engl J Med. 2002; 347:240–247.
Article10. Jeon GW, Sin JB. Risk factors of transfusion in anemia of very low birth weight infants. Yonsei Med J. 2013; 54:366–373.
Article11. Eschenbach DA. Amniotic fluid infection and cerebral palsy. Focus on the fetus. JAMA. 1997; 278:247–248.
Article12. Bender L, Thaarup J, Varming K, Krarup H, Ellermann-Eriksen S, Ebbesen F. Early and late markers for the detection of early-onset neonatal sepsis. Dan Med Bull. 2008; 55:219–223.13. Hirsch W, Koppitz D, Morack G, Gerhardt C. [C-reactive protein in the maternal serum and risk of fetal infection in premature rupture of the fetal membranes and threatened premature labor]. Zentralbl Gynakol. 1989; 111:1411–1416.14. Skrablin S, Lovric H, Banovic V, Kralik S, Dijakovic A, Kalafatic D. Maternal plasma interleukin-6, interleukin-1beta and C-reactive protein as indicators of tocolysis failure and neonatal outcome after preterm delivery. J Matern Fetal Neonatal Med. 2007; 20:335–341.15. van der Heyden JL, van Teeffelen SS, Coolen AC, Halbertsma FJ, Aardenburg R, Mertens HJ, et al. Is it useful to measure C-reactive protein and leukocytes in patients with prelabor rupture of membranes? Am J Perinatol. 2010; 27:543–547.
Article16. Trochez-Martinez RD, Smith P, Lamont RF. Use of C-reactive protein as a predictor of chorioamnionitis in preterm prelabour rupture of membranes: a systematic review. BJOG. 2007; 114:796–801.
Article17. Mehr SS, Sadowsky JL, Doyle LW, Carr J. Sepsis in neonatal intensive care in the late 1990s. J Paediatr Child Health. 2002; 38:246–251.
Article18. Young Infants Clinical Signs Study Group. Clinical signs that predict severe illness in children under age 2 months: a multicentre study. Lancet. 2008; 371:135–142.19. NICE clinical guidesines. CG Antibiotics for early-onset neonatal infection: antibiotics for the prevention and treatment of early-onset neonatal infection. Manchester: National Institute for Health and Clinical Excellence;2012.20. Edmond K, Zaidi A. New approaches to preventing, diagnosing, and treating neonatal sepsis. PLoS Med. 2010; 7:e1000213.
Article21. Yoon BH, Romero R, Kim CJ, Jun JK, Gomez R, Choi JH, et al. Amniotic fluid interleukin-6: a sensitive test for antenatal diagnosis of acute inflammatory lesions of preterm placenta and prediction of perinatal morbidity. Am J Obstet Gynecol. 1995; 172:960–970.
Article22. Beck JR, Shultz EK. The use of relative operating characteristic (ROC) curves in test performance evaluation. Arch Pathol Lab Med. 1986; 110:13–20.23. Irwin RJ, Irwin TC. A principled approach to setting optimal diagnostic thresholds: where ROC and indifference curves meet. Eur J Intern Med. 2011; 22:230–234.
Article24. Zimmerman MA, Selzman CH, Cothren C, Sorensen AC, Raeburn CD, Harken AH. Diagnostic implications of C-reactive protein. Arch Surg. 2003; 138:220–224.
Article25. Picklesimer AH, Jared HL, Moss K, Offenbacher S, Beck JD, Boggess KA. Racial differences in C-reactive protein levels during normal pregnancy. Am J Obstet Gynecol. 2008; 199:523.
Article26. Yoon BH, Jun JK, Park KH, Syn HC, Gomez R, Romero R. Serum C-reactive protein, white blood cell count, and amniotic fluid white blood cell count in women with preterm premature rupture of membranes. Obstet Gynecol. 1996; 88:1034–1040.
Article27. Pfeiffer KA, Reinsberg J, Rahmun A, Schmolling J, Krebs D. Clinical application of maternal serum cytokine determination in premature rupture of membranes--interleukin-6, an early predictor of neonatal infection? Acta Obstet Gynecol Scand. 1999; 78:774–778.
Article28. Celik IH, Demirel FG, Uras N, Oguz SS, Erdeve O, Biyikli Z, et al. What are the cut-off levels for IL-6 and CRP in neonatal sepsis? J Clin Lab Anal. 2010; 24:407–412.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prenatal Diagnosis of Intrauterine Infection and Prediction of Neonatal Morbidity by Maternal Serum C-Reactive Protein in Patients with Preterm Premature Rupture of Membranes
- Management of Newborns of Mothers with the Premature Rupture of Membranes
- The Diagnostic and Prognostic Value of Maternal Blood C-reactive Protein in Patients with Preterm Labor and Intact Membranes
- Comparison of the accuracy of neutrophil CD64 and C-reactive protein as a single test for the early detection of neonatal sepsis
- Diagnostic and prognostic value of proadrenomedullin in neonatal sepsis