Yonsei Med J.
2014 Jan;55(1):37-45. 10.3349/ymj.2014.55.1.37.
Prognosis after Implantation of Cardioverter-Defibrillators in Korean Patients with Brugada Syndrome
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Cardiac and Vascular Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. yk.on@samsung.com
- 2Division of Cardiology, Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 3Division of Cardiology, Department of Internal Medicine, Korea University Cardiovascular Center, Korea University College of Medicine, Seoul, Korea.
- 4Heart Research Center, Chonnam National University Hospital, Chonnam National University, Gwangju, Korea.
- KMID: 1779884
- DOI: http://doi.org/10.3349/ymj.2014.55.1.37
Abstract
- PURPOSE
Our study aims to analyze prognosis after implantable cardioverter-defibrillator (ICD) implantation in Korean patients with Brugada syndrome (BrS).
MATERIALS AND METHODS
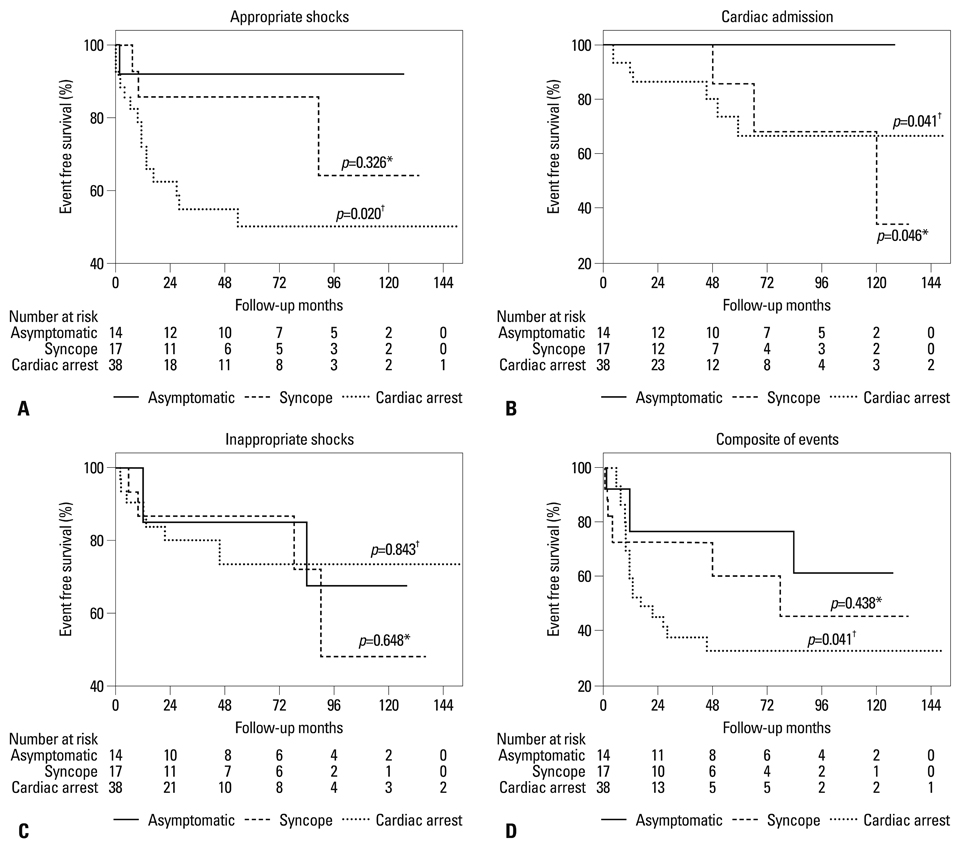
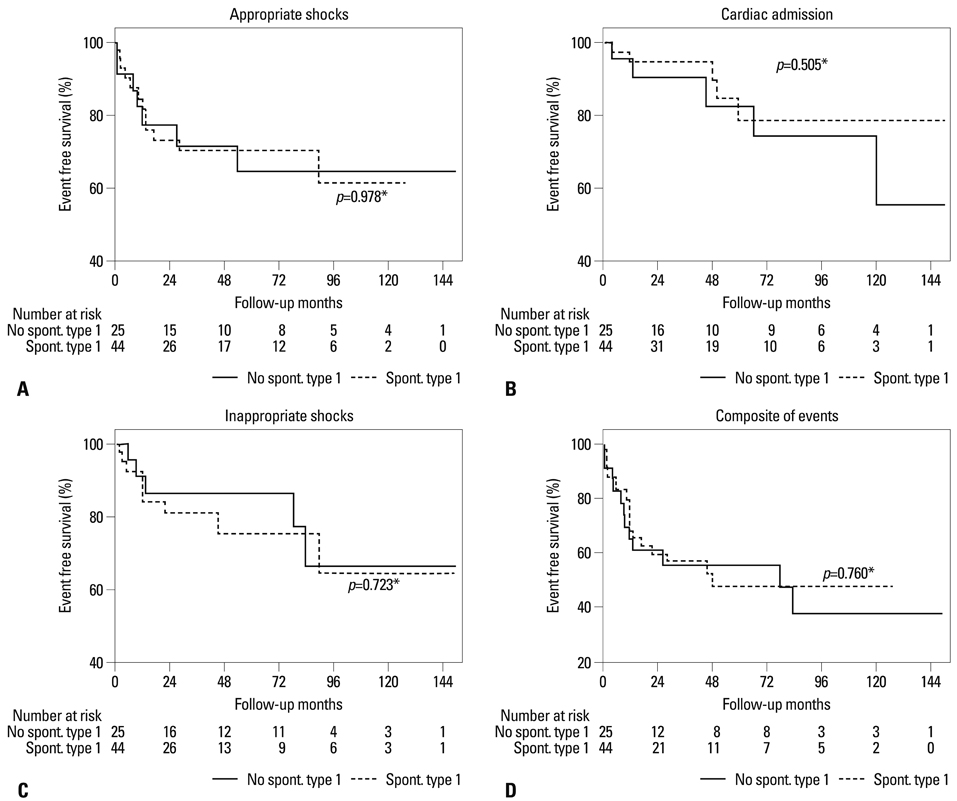
This was a retrospective study of BrS patients implanted with an ICD at one of four centers in Korea between January 1998 and April 2012. Sixty-nine patients (68 males, 1 female) were implanted with an ICD based on aborted cardiac arrest (n=38, 55%), history of syncope (n=17, 25%), or induced ven tricular tachyarrhythmia on electrophysiologic study in asymptomatic patients (n=14, 20%). A family history of sudden cardiac death and a spontaneous type 1 electrocardiography (ECG) were noted in 13 patients (19%) and 44 patients (64%), respectively.
RESULTS
During a mean follow-up of 59+/-46 months, 4.6+/-5.5 appropri ate shocks were delivered in 19 patients (28%). Fourteen patients (20%) experienced 5.2+/-8.0 inappropriate shocks caused by supraventricular arrhythmia, lead failure, or abnormal sensing. Six patients were admitted for cardiac causes during follow-up, but no cardiac deaths occurred. An episode of aborted cardiac arrest was a significant predictor of appropriate shock, and the composite of cardiac events in the Cox pro portional hazard model [hazard ratio (95% confidence interval) was 11.34 (1.31-97.94) and 4.78 (1.41-16.22), respectively]. However, a spontaneous type 1 ECG was not a predictor of cardiac events.
CONCLUSION
Appropriate shock (28%) and inappropriate shock (20%) were noted during a mean follow-up of 59+/-46 months in Korean BrS patients implanted with an ICD. An episode of aborted cardiac ar rest was the most powerful predictor of cardiac events.
MeSH Terms
Figure
Reference
-
1. Mizusawa Y, Wilde AA. Brugada syndrome. Circ Arrhythm Electrophysiol. 2012; 5:606–616.
Article2. Berne P, Brugada J. Brugada syndrome 2012. Circ J. 2012; 76:1563–1571.
Article3. Sarkozy A, Boussy T, Kourgiannides G, Chierchia GB, Richter S, De Potter T, et al. Long-term follow-up of primary prophylactic implantable cardioverter-defibrillator therapy in Brugada syndrome. Eur Heart J. 2007; 28:334–344.
Article4. Sacher F, Probst V, Iesaka Y, Jacon P, Laborderie J, Mizon-Gérard F, et al. Outcome after implantation of a cardioverter-defibrillator in patients with Brugada syndrome: a multicenter study. Circulation. 2006; 114:2317–2324.
Article5. Eckardt L, Probst V, Smits JP, Bahr ES, Wolpert C, Schimpf R, et al. Long-term prognosis of individuals with right precordial ST-segment-elevation Brugada syndrome. Circulation. 2005; 111:257–263.
Article6. Priori SG, Napolitano C, Gasparini M, Pappone C, Della Bella P, Giordano U, et al. Natural history of Brugada syndrome: insights for risk stratification and management. Circulation. 2002; 105:1342–1347.
Article7. Gehi AK, Duong TD, Metz LD, Gomes JA, Mehta D. Risk stratification of individuals with the Brugada electrocardiogram: a meta-analysis. J Cardiovasc Electrophysiol. 2006; 17:577–583.
Article8. Probst V, Veltmann C, Eckardt L, Meregalli PG, Gaita F, Tan HL, et al. Long-term prognosis of patients diagnosed with Brugada syndrome: results from the FINGER Brugada Syndrome Registry. Circulation. 2010; 121:635–643.
Article9. Wilde AA, Antzelevitch C, Borggrefe M, Brugada J, Brugada R, Brugada P, et al. Proposed diagnostic criteria for the Brugada syndrome: consensus report. Circulation. 2002; 106:2514–2519.
Article10. European Heart Rhythm Association. Heart Rhythm Society. Zipes DP, Camm AJ, Borggrefe M, Buxton AE, et al. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death). J Am Coll Cardiol. 2006; 48:e247–e346.11. Priori SG, Gasparini M, Napolitano C, Della Bella P, Ottonelli AG, Sassone B, et al. Risk stratification in Brugada syndrome: results of the PRELUDE (PRogrammed ELectrical stimUlation preDictive valuE) registry. J Am Coll Cardiol. 2012; 59:37–45.12. Sacher F, Arsac F, Wilton SB, Derval N, Denis A, de Guillebon M, et al. Syncope in Brugada syndrome patients: prevalence, characteristics, and outcome. Heart Rhythm. 2012; 9:1272–1279.
Article13. Take Y, Morita H, Toh N, Nishii N, Nagase S, Nakamura K, et al. Identification of high-risk syncope related to ventricular fibrillation in patients with Brugada syndrome. Heart Rhythm. 2012; 9:752–759.
Article14. Richter S, Sarkozy A, Veltmann C, Chierchia GB, Boussy T, Wolpert C, et al. Variability of the diagnostic ECG pattern in an ICD patient population with Brugada syndrome. J Cardiovasc Electrophysiol. 2009; 20:69–75.
Article15. Veltmann C, Schimpf R, Echternach C, Eckardt L, Kuschyk J, Streitner F, et al. A prospective study on spontaneous fluctuations between diagnostic and non-diagnostic ECGs in Brugada syndrome: implications for correct phenotyping and risk stratification. Eur Heart J. 2006; 27:2544–2552.
Article16. Ikeda T, Abe A, Yusu S, Nakamura K, Ishiguro H, Mera H, et al. The full stomach test as a novel diagnostic technique for identifying patients at risk of Brugada syndrome. J Cardiovasc Electrophysiol. 2006; 17:602–607.
Article17. Di Diego JM, Cordeiro JM, Goodrow RJ, Fish JM, Zygmunt AC, Pérez GJ, et al. Ionic and cellular basis for the predominance of the Brugada syndrome phenotype in males. Circulation. 2002; 106:2004–2011.
Article18. Zorzi A, Migliore F, Marras E, Marinelli A, Baritussio A, Allocca G, et al. Should all individuals with a nondiagnostic Brugada-electrocardiogram undergo sodium-channel blocker test? Heart Rhythm. 2012; 9:909–916.
Article19. Nishizaki M, Sakurada H, Yamawake N, Ueda-Tatsumoto A, Hiraoka M. Low risk for arrhythmic events in asymptomatic patients with drug-induced type 1 ECG. Do patients with drug-induced Brugada type ECG have poor prognosis? (Con). Circ J. 2010; 74:2464–2473.
Article20. Lee YS, Baek JS, Kim SY, Seo SW, Kwon BS, Kim GB, et al. Childhood brugada syndrome in two korean families. Korean Circ J. 2010; 40:143–147.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intrapericardial Implantation of an Implantable Cardioverter-Defibrillator in a Child
- Anesthetic Experience of Appendectomy of a Patient with Implantable Cardioverter Defibrillator: A case report
- Brugada Syndrome
- Transvenous Implantation of an Implantable Cardioverter Defibrillator in a Patient Who Had Undergone Tricuspid Valve Replacement
- Clinical characteristics of patients with an implantable cardioverter-defibrillator: Our experience at Asan Medical Center