Yonsei Med J.
2010 Nov;51(6):938-942. 10.3349/ymj.2010.51.6.938.
Schwannoma in Head and Neck: Preoperative Imaging Study and Intracapsular Enucleation for Functional Nerve Preservation
- Affiliations
-
- 1Department of Otorhinolaryngology, Institute of Logopedics & Phoniatrics, Yonsei University College of Medicine, Gangnam Severance Hospital, Seoul, Korea. hschoi@yuhs.ac
- KMID: 1779643
- DOI: http://doi.org/10.3349/ymj.2010.51.6.938
Abstract
- PURPOSE
In treating schwannoma patients, it is critical to determine the origin of the tumor to preserve nerve function. We evaluated the validity of preoperative imaging studies in distinguishing the neurological origin of the schwannomas of the head and neck, and the efficacy of intracapsular enucleation in preserving nerve function.
MATERIALS AND METHODS
In 7 cases of schwannomas in the head and neck region, we predicted whether the tumor originated from the vagus nerve or the cervical sympathetic chain through imaging studies including computed tomography (CT) and magnetic resonance imaging (MRI). All patients were performed intracapsular enucleation, and the function of the vagus nerve and the sympathetic nerve was evaluated preoperatively and postoperatively.
RESULTS
Preoperative imaging studies showed 6 cases where the tumor was located between the carotid artery and the internal jugular vein, and 1 case where the tumor was located posteriorly, displacing the carotid artery and the internal jugular vein anteriorly. At the time of operation, we confirmed schwannoma originating from the vagus nerve on the first 6 cases, and schwannoma originating from the sympathetic nervous system on the last case. All patients went through successful intracapsular enucleation, and of the seven schwannoma cases, 6 patients maintained normal postoperative neurological function (85.7%).
CONCLUSION
Preoperative imaging studies offer valuable information regarding the location and origination of the tumor, and intracapsular enucleation helped us to preserve the nerve function.
MeSH Terms
-
Aged
Diagnostic Imaging/methods
Female
Follow-Up Studies
Head and Neck Neoplasms/complications/diagnosis/*pathology
Humans
Magnetic Resonance Imaging/methods
Male
Middle Aged
Neurilemmoma/complications/diagnosis/*pathology
Peripheral Nervous System/injuries/physiology
Sympathetic Nervous System/physiology
Tomography, X-Ray Computed/methods
Treatment Outcome
Vagus Nerve/physiology
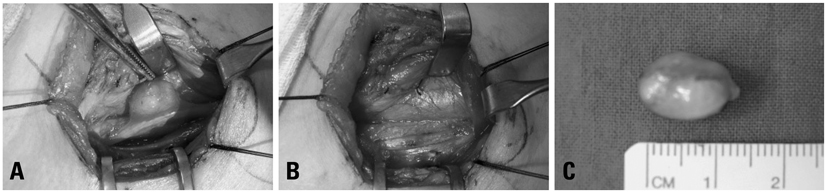
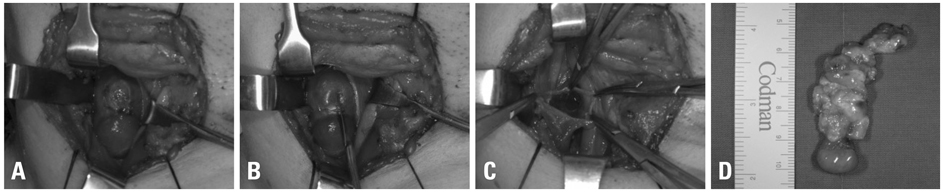
Figure
Cited by 1 articles
-
Ansa cervicalis: a comprehensive review of its anatomy, variations, pathology, and surgical applications
Shogo Kikuta, Skyler Jenkins, Jingo Kusukawa, Joe Iwanaga, Marios Loukas, R. Shane Tubbs
Anat Cell Biol. 2019;52(3):221-225. doi: 10.5115/acb.19.041.
Reference
-
1. Ducatman BS, Scheithauer BW, Piepgras DG, Reiman HM, Ilstrup DM. Malignant peripheral nerve sheath tumors. A clinicopathologic study of 120 cases. Cancer. 1986. 57:2006–2021.
Article2. Colreavy MP, Lacy PD, Hughes J, Bouchier-Hayes D, Brennan P, O'Dwyer AJ, et al. Head and neck schwannomas: a 10 year review. J Laryngol Otol. 2000. 114:119–124.3. Furukawa M, Furukawa MK, Katoh K, Tsukuda M. Differentiation between schwannoma of the vagus nerve and schwannoma of the cervical sympathetic chain by imaging diagnosis. Laryngoscope. 1996. 106:1548–1552.
Article4. Fujino K, Shinohara K, Aoki M, Hashimoto K, Omori K. Intracapsular enucleation of vagus nerve-originated tumors for preservation of neural function. Otolaryngol Head Neck Surg. 2000. 123:334–336.
Article5. Fornaro R, Frascio M, Stabilini C. Excision of a schwannoma of the head and neck: surgical technique. G Chir. 2006. 27:428–432.6. Moukarbel RV, Sabri AN. Current management of head and neck schwannomas. Curr Opin Otolaryngol Head Neck Surg. 2005. 13:117–122.
Article7. Wax MK, Shiley SG, Robinson JL, Weissman JL. Cervical sympathetic chain schwannoma. Laryngoscope. 2004. 114:2210–2213.
Article8. Gilmer-Hill HS, Kline DG. Neurogenic tumors of the cervical vagus nerve: report of four cases and review of the literature. Neurosurgery. 2000. 46:1498–1503.
Article9. de Araujo CE, Ramos DM, Moyses RA, Durazzo MD, Cernea CR, Ferraz AR. Neck nerve trunks schwannomas: clinical features and postoperative neurologic outcome. Laryngoscope. 2008. 118:1579–1582.
Article10. Wang CP, Hsiao JK, Ko JY. Splaying of the carotid bifurcation caused by a cervical sympathetic chain schwannoma. Ann Otol Rhinol Laryngol. 2004. 113:696–699.11. Miller FR, Wanamaker JR, Lavertu P, Wood BG. Magnetic resonance imaging and the management of parapharyngeal space tumors. Head Neck. 1996. 18:67–77.
Article12. Saito DM, Glastonbury CM, El-Sayed IH, Eisele DW. Parapharyngeal space schwannomas: preoperative imaging determination of the nerve of origin. Arch Otolaryngol Head Neck Surg. 2007. 133:662–667.13. Chang SC, Schi YM. Neurilemmoma of the vagus nerve. A case report and brief literature review. Laryngoscope. 1984. 94:946–949.
Article14. Saydam L, Kizilay A, Kalcioglu T, Gurer I. Ancient cervical vagal neurilemmoma: a case report. Am J Otolaryngol. 2000. 21:61–64.
Article15. Valentino J, Boggess MA, Ellis JL, Hester TO, Jones RO. Expected neurologic outcomes for surgical treatment of cervical neurilemomas. Laryngoscope. 1998. 108:1009–1013.
Article16. Charles D, Yingling CD. Cummings CW, Fredrickson JM, Harker LA, Krause CJ, Schuller DE, editors. Intraoperative monitoring of cranial nerves in neurotologic surgery. Otolaryngol-Head and Neck Surgery. 1996. St. Louis: Mosby year Book;3331–3355.17. Pesavento G, Ferlito A, Recher G. Benign solitary schwannoma of the cervical vagus nerve. A case report with a review of the literature. J Laryngol Otol. 1979. 93:307–316.18. Langner E, Del Negro A, Akashi HK, Araújo PP, Tincani AJ, Martins AS. Schwannomas in the head and neck: retrospective analysis of 21 patients and review of the literature. Sao Paulo Med J. 2007. 125:220–222.
Article19. Zbären P, Markwalder R. Schwannoma of the true vocal cord. Otolaryngol Head Neck Surg. 1999. 121:837–839.
Article