Yonsei Med J.
2010 Nov;51(6):823-831. 10.3349/ymj.2010.51.6.823.
Comparisons of the Effects of Stent Eccentricity on the Neointimal Hyperplasia between Sirolimus-Eluting Stent versus Paclitaxel-Eluting Stent
- Affiliations
-
- 1Division of Cardiology, Cardiovascular Center, National Health Insurance Corporation Ilsan Hospital, Goyang, Korea.
- 2Division of Cardiology, Yonsei Cardiovascular Center, Yonsei University College of Medicine, Seoul, Korea. jangys1212@yuhs.ac
- 3Division of Cardiology, Gachon University of Medicine and Science, Incheon, Korea.
- KMID: 1779626
- DOI: http://doi.org/10.3349/ymj.2010.51.6.823
Abstract
- PURPOSE
Previous studies suggested that asymmetric stent expansion did not affect suppression of neointimal hyperplasia (NIH) after sirolimus-eluting stents (SES) implantation. The aim of this study was to evaluate the effects of stent eccentricity (SE) on NIH between SES versus paclitaxel-eluting stents (PES) using an intravascular ultrasound (IVUS) analysis from the randomized trial.
MATERIALS AND METHODS
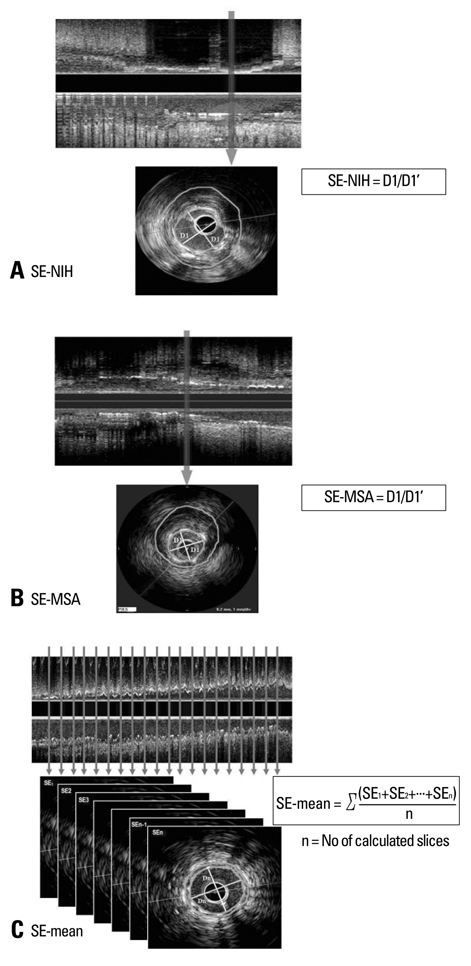
Serial IVUS data were obtained from Post-stent Optimal Expansion (POET) trial, allocated randomly to SES or PES. Three different SE (minimum stent diameter divided by maximum stent diameter) were evaluated; SE at the lesion site with maximal %NIH area (SE-NIH), SE at the minimal stent CSA [SE-minimal stent area (SE-MSA)], and averaged SE through the entire stent (SE-mean). We classified each drug-eluting stents (DES) into the concentric (> or = mean SE) and eccentric groups (< mean SE) based on the mean value of SE.
RESULTS
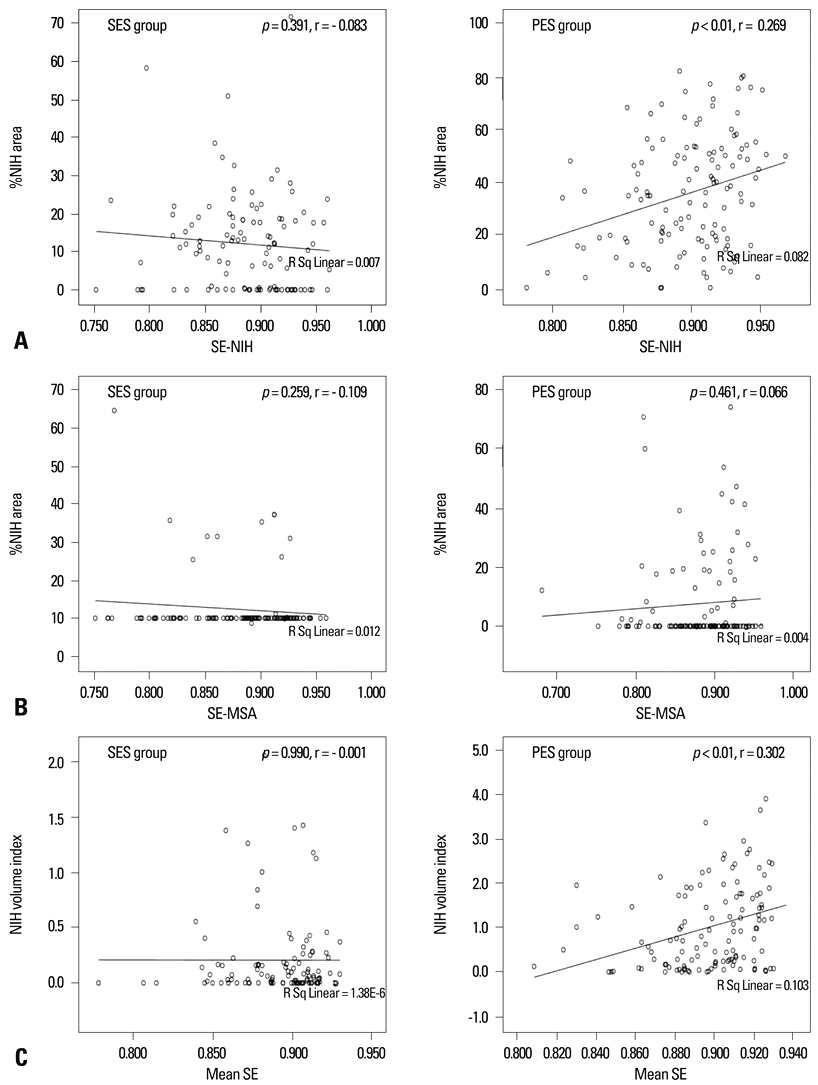
Among 301 enrolled patients, 233 patients [SES (n = 108), PES (n = 125)] underwent a follow-up IVUS. There was no significant correlation between %NIH area and SE-NIH (r = - 0.083, p = 0.391) or SE-MSA (r = - 0.109, p = 0.259) of SES. However, SE-NIH of PES showed a weak but significant correlation with %NIH area (r = 0.269, p < 0.01). As to the associations between SE-mean and NIH volume index, SES revealed no significant correlation (r = - 0.001, p = 0.990), but PES showed a weak but significant correlation (r = 0.320, p < 0.01). However, there was no difference in the restenosis rate between the eccentric versus concentric groups of both DES.
CONCLUSION
This study suggests that lower SE of both SES and PES, which means asymmetric stent expansion, may not be associated with increased NIH.
MeSH Terms
-
Aged
Angiography/methods
Coronary Restenosis/pathology/ultrasonography
*Drug-Eluting Stents
Female
Humans
Hyperplasia/*drug therapy/pathology
Immunosuppressive Agents/administration & dosage
Male
Middle Aged
Paclitaxel/*administration & dosage
Sirolimus/*administration & dosage
Tunica Intima
Ultrasonography, Interventional/methods
Figure
Cited by 1 articles
-
Comparison of Optical Coherence Tomographic Assessment between First- and Second-Generation Drug-Eluting Stents
Byeong-Keuk Kim, Jung-Sun Kim, Junbeom Park, Young-Guk Ko, Donghoon Choi, Yangsoo Jang, Myeong-Ki Hong
Yonsei Med J. 2012;53(3):524-529. doi: 10.3349/ymj.2012.53.3.524.
Reference
-
1. Kataoka T, Grube E, Honda Y, Morino Y, Hur SH, Bonneau HN, et al. 7-hexanoyltaxol-eluting stent for prevention of neointimal growth: an intravascular ultrasound analysis from the Study to COmpare REstenosis rate between QueST and QuaDS-QP2 (SCORE). Circulation. 2002. 106:1788–1793.
Article2. Park SJ, Shim WH, Ho DS, Raizner AE, Park SW, Hong MK, et al. A paclitaxel-eluting stent for the prevention of coronary restenosis. N Engl J Med. 2003. 348:1537–1545.
Article3. Lambert TL, Dev V, Rechavia E, Forrester JS, Litvack F, Eigler NL. Localized arterial wall drug delivery from a polymer-coated removable metallic stent. Kinetics, distribution, and bioactivity of forskolin. Circulation. 1994. 90:1003–1011.
Article4. Hwang CW, Wu D, Edelman ER. Physiological transport forces govern drug distribution for stent-based delivery. Circulation. 2001. 104:600–605.
Article5. Lansky AJ, Costa RA, Mintz GS, Tsuchiya Y, Midei M, Cox DA, et al. Non-polymer-based paclitaxel-coated coronary stents for the treatment of patients with de novo coronary lesions: angiographic follow-up of the DELIVER clinical trial. Circulation. 2004. 109:1948–1954.6. Moses JW, Leon MB, Popma JJ, Fitzgerald PJ, Holmes DR, O'Shaughnessy C, et al. Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N Engl J Med. 2003. 349:1315–1323.
Article7. Kaneda H, Ako J, Honda Y, Terashima M, Morino Y, Yock PG, et al. Impact of asymmetric stent expansion on neointimal hyperplasia following sirolimus-eluting stent implantation. Am J Cardiol. 2005. 96:1404–1407.
Article8. Kim JS, Moon JY, Ko YG, Choi D, Jang Y, Kang WC, et al. Intravascular ultrasound evaluation of optimal drug-eluting stent expansion after poststent balloon dilation using a noncompliant balloon versus a semicompliant balloon (from the Poststent Optimal Stent Expansion Trial [POET]). Am J Cardiol. 2008. 102:304–310.
Article9. de Jaegere P, Mudra H, Figulla H, Almagor Y, Doucet S, Penn I, et al. Intravascular ultrasound-guided optimized stent deployment. Immediate and 6 months clinical and angiographic results from the Multicenter Ultrasound Stenting in Coronaries Study (MUSIC Study). Eur Heart J. 1998. 19:1214–1223.
Article10. Nakano M, Wagatsuma K, Iga A, Nii H, Amano H, Toda M, et al. Impact of highly asymmetric stent expansion after sirolimus-eluting stent implantation on twelve-month clinical outcomes. J Cardiol. 2007. 49:313–321.11. Mintz GS, Weissman NJ. Intravascular ultrasound in the drug-eluting stent era. J Am Coll Cardiol. 2006. 48:421–429.
Article12. Sonoda S, Morino Y, Ako J, Terashima M, Hassan AH, Bonneau HN, et al. Impact of final stent dimensions on long-term results following sirolimus-eluting stent implantation: serial intravascular ultrasound analysis from the Sirius trial. J Am Coll Cardiol. 2004. 43:1959–1963.
Article13. Hong MK, Mintz GS, Lee CW, Park DW, Choi BR, Park KH, et al. Intravascular ultrasound predictors of angiographic restenosis after sirolimus-eluting stent implantation. Eur Heart J. 2006. 27:1305–1310.14. Takebayashi H, Mintz GS, Carlier SG, Kobayashi Y, Fujii K, Yasuda T, et al. Nonuniform strut distribution correlates with more neointimal hyperplasia after sirolimus-eluting stent implantation. Circulation. 2004. 110:3430–3434.15. Hasegawa T, Ako J, Ikeno F, Waseda K, Suzuki Y, Honda Y, et al. Comparison of nonuniform strut distribution between two drug-eluting stent platforms. J Invasive Cardiol. 2007. 19:244–246.16. Opolski MP, Pracon R, Mintz GS, Weissman NJ, Mandinov L, Pregowski J, et al. Stent strut distribution at implantation and 9-month follow-up in TAXUS and bare metal stents and its effect on neointimal hyperplasia. J Am Coll Cardiol. 2009. 53:A9.17. Otake H, Shite J, Ako J, Shinke T, Tanino Y, Ogasawara D, et al. Local determinants of thrombus formation following sirolimus-eluting stent implantation assessed by optical coherence tomography. JACC Cardiovasc Interv. 2009. 2:459–466.
Article18. Kim U, Kim JS, Kim JS, Lee JM, Son JW, Kim J, et al. The initial extent of malapposition in ST-elevation myocardial infarction treated with drug-eluting stent: the usefulness of optical coherence tomography. Yonsei Med J. 2010. 51:332–338.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Very Late Stent Thrombosis Related to Fracture of a Sirolimus-Eluting Stent
- A Case of Neointimal Calcification in a Drug-Eluting Stent
- A Case of Stent Strut Fracture of a Paclitaxel-Eluting Stent at the Time of Stent Implantation in a Complex Coronary Lesion
- Drug-Eluting Stent Strut Fracture as a Cause of Restenosis
- Late Stent Thrombosis Associated with Late Stent Malapposition after Drug-Eluting Stenting: A Case Report