Korean J Radiol.
2007 Jun;8(3):236-241. 10.3348/kjr.2007.8.3.236.
Anterior Cruciate Ligament Tear: Reliability of MR Imaging to Predict Stability after Conservative Treatment
- Affiliations
-
- 1Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. chung@amc.seoul.kr
- 2Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 3Department of Orthopaedic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Department of Radiology, University of Iowa Hospital and Clinics, USA.
- 5Biostatistics Unit of the Samsung Biomedical Research Institute of Samsung Medical Center, Seoul , Korea.
- KMID: 1779440
- DOI: http://doi.org/10.3348/kjr.2007.8.3.236
Abstract
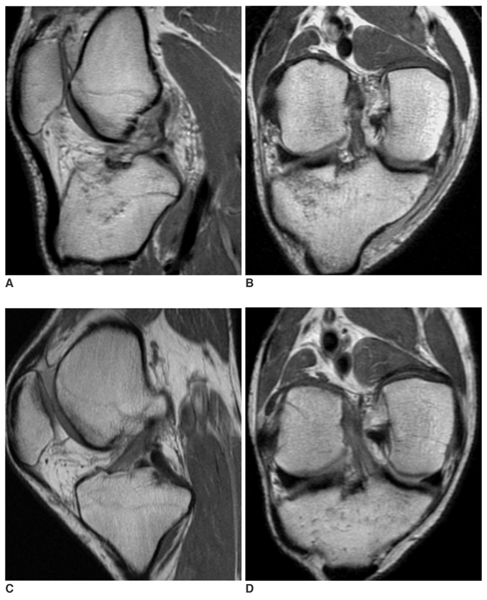
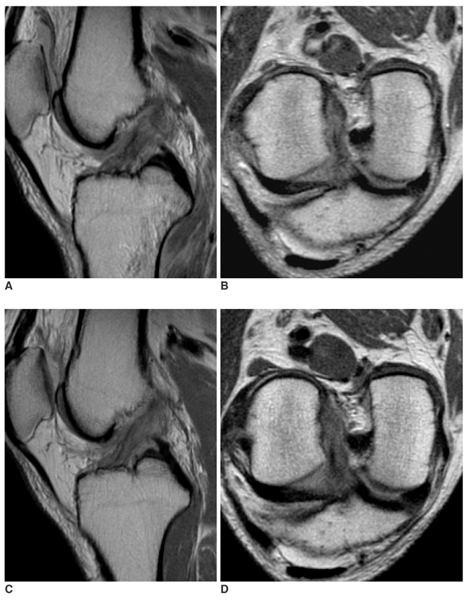
OBJECTIVE
The aim of this study is to evaluate the reliability of MR imaging to predict the stability of the torn anterior cruciate ligament (ACL) after complete recovery of the ligament's continuity. MATERIALS AND METHODS: Twenty patients with 20 knee injuries (13 males and 7 females; age range, 20-54) were enrolled in the study. The inclusion criteria were a positive history of acute trauma, diagnosis of the ACL tear by both the physical examination and the MR imaging at the initial presentation, conservative treatment, complete recovery of the continuity of the ligament on the follow up (FU) MR images and availability of the KT-2000 measurements. Two radiologists, who worked in consensus, graded the MR findings with using a 3-point system for the signal intensity, sharpness, straightness and the thickness of the healed ligament. The insufficiency of ACL was categorized into three groups according to the KT-2000 measurements. The statistic correlations between the grades of the MR findings and the degrees of ACL insufficiency were analyzed using the Cochran-Mantel-Haenszel test (p < 0.05). RESULTS: The p-values for each category of the MR findings according to the different groups of the KT-2000 measurements were 0.9180 for the MR signal intensity, 1.0000 for sharpness, 0.5038 for straightness and 0.2950 for thickness of the ACL. The MR findings were not significantly different between the different KT-2000 groups. CONCLUSION: MR imaging itself is not a reliable examination to predict stability of the ACL rupture outcome, even when the MR images show an intact appearance of the ACL.
Keyword
MeSH Terms
Figure
Reference
-
1. Fujimoto E, Sumen Y, Ochi M, Ikuta Y. Spontaneous healing of acute anterior cruciate ligament (ACL) injuries - conservative treatment using an extension block soft brace without anterior stabilization. Arch Orthop Trauma Surg. 2002. 122:212–216.2. Higueras Guerrero V, Torregrosa Andres A, Marti-Bonmati L, Casillas C, Sanfeliu M. Synovialisation of the torn anterior cruciate ligament of the knee: comparison between magnetic resonance and arthroscopy. Eur Radiol. 1999. 9:1796–1799.3. Ihara H, Miwa M, Deya K, Torisu K. MRI of anterior cruciate ligament healing. J Comput Assist Tomogr. 1996. 20:317–321.4. Malanga GA, Giradi J, Nadler SF. The spontaneous healing of a torn anterior cruciate ligament. Clin J Sport Med. 2001. 11:118–120.5. Frank CB. Ligament structure, physiology and function. J Musculoskelet Neuronal Interact. 2004. 4:199–201.6. Daniel DM, Malcom LL, Losse G, Stone ML, Sachs R, Burks R. Instrumented measurement of anterior laxity of the knee. J Bone Joint Surg Am. 1985. 67:720–726.7. Arnoczky SP, Rubin RM, Marshall JL. Microvasculature of the cruciate ligaments and its response to injury. An experimental study in dogs. J Bone Joint Surg Am. 1979. 61:1221–1229.8. Bray RC, Leonard CA, Salo PT. Correlation of healing capacity with vascular response in the anterior cruciate and medial collateral ligaments of the rabbit. J Orthop Res. 2003. 21:1118–1123.9. Andersson C, Odensten M, Good L, Gillquist J. Surgical or non-surgical treatment of acute rupture of the anterior cruciate ligament. A randomized study with long-term follow-up. J Bone Joint Surg Am. 1989. 71:965–974.10. Hefti FL, Kress A, Fasel J, Morscher EW. Healing of the transected anterior cruciate ligament in the rabbit. J Bone Joint Surg Am. 1991. 73:373–383.11. Noyes FR, Mooar PA, Matthews DS, Butler DL. The symptomatic anterior cruciate-deficient knee. Part I: the long-term functional disability in athletically active individuals. J Bone Joint Surg Am. 1983. 65:154–162.12. Noyes FR, Matthews DS, Mooar PA, Grood ES. The symptomatic anterior cruciate-deficient knee. Part II: the results of rehabilitation, activity modification, and counseling on functional disability. J Bone Joint Surg Am. 1983. 65:163–174.13. Fujimoto E, Sumen Y, Deie M, Yasumoto M, Kobayashi K, Ochi M. Anterior cruciate ligament graft impingement against the posterior cruciate ligament: diagnosis using MRI plus three-dimensional reconstruction software. Magn Reson Imaging. 2004. 22:1125–1129.14. Tung GA, Davis LM, Wiggins ME, Fadale PD. Tears of the anterior cruciate ligament: primary and secondary signs at MR imaging. Radiology. 1993. 188:661–667.15. Lee JK, Yao L, Phelps CT, Wirth CR, Czajka J, Lozman J. Anterior cruciate ligament tears: MR imaging compared with arthroscopy and clinical tests. Radiology. 1988. 166:861–864.16. Farley TE, Howell SM, Love KF, Wolfe RD, Neumann CH. Meniscal tears: MR and arthrographic findings after arthroscopic repair. Radiology. 1991. 180:517–522.17. Steenbrugge F, Verstraete K, Verdonk R. Magnetic reasonance imaging of the surgically repaired meniscus: a 13-year follow-up study of 13 knees. Acta Orthop Scand. 2004. 75:323–327.18. Yamato M, Yamagishi T. MRI of patellar tendon anterior cruciate ligament autografts. J Comput Assist Tomogr. 1992. 16:604–607.19. Cheung Y, Magee TH, Rosenberg ZS, Rose DJ. MRI of anterior cruciate ligament reconstruction. J Comput Assist Tomogr. 1992. 16:134–137.20. von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis. 2004. 63:269–273.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Tears of the Anterior Cruciate Ligament:Analysis of the Tear Site and the Degree Using MR Imaging
- Indirect Signs of Magnetic Resonance Imaging of the Knee with Anterior Cruciate Ligament Tears: Comparison between Acute and Chronic ACL Tears
- The Primary Repair of Acute Anterior Cruciate Ligament Injury
- Acute and Chronic Tears of Anterior Cruciate Ligament: Role of Gadolinium-enhanced MR Imaging
- Indirect signs of anterior cruciate ligament injuries at mr imaging