J Korean Med Sci.
2009 Jun;24(3):461-467. 10.3346/jkms.2009.24.3.461.
Neuroblastoma Originating from Extra-abdominal Sites: Association with Favorable Clinical and Biological Features
- Affiliations
-
- 1Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Thoracic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jkimsmc@skku.edu
- 4Department of Pediatric Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. sklee3464@skku.edu
- KMID: 1779164
- DOI: http://doi.org/10.3346/jkms.2009.24.3.461
Abstract
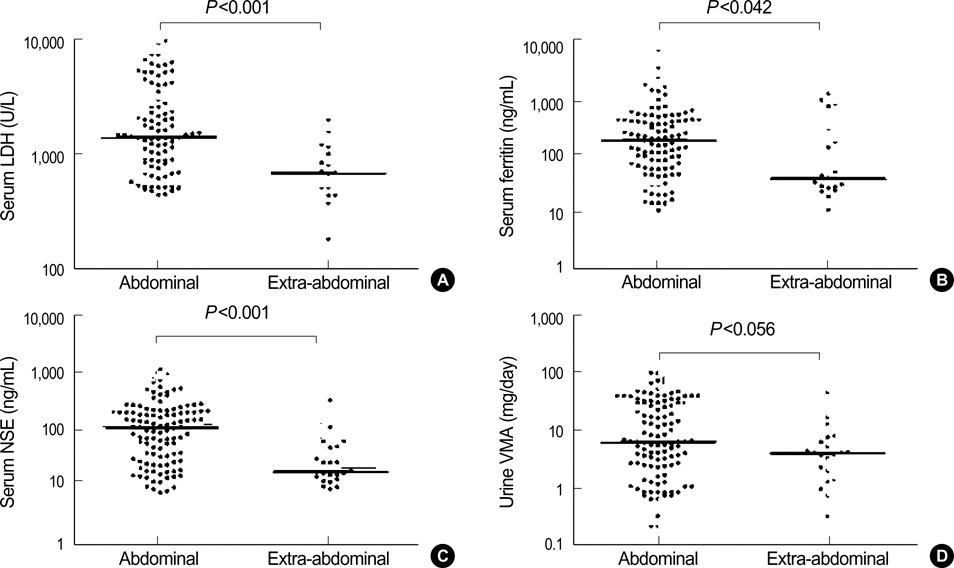
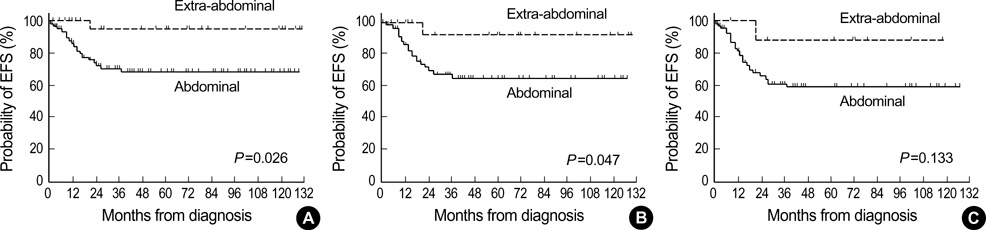
- Neuroblastomas originating from different sites might have different clinical and biological characteristics. In the present study, the clinical (age, sex and stage) and biological (N-myc amplification, Shimada pathology and levels of lactate dehydrogenase, ferritin and neuron-specific enolase) characteristics of patients with newly diagnosed neuroblastoma were compared according to the site of tumor origin (extra-abdominal versus abdominal). The event-free survival rate (EFS) was also compared between the two groups. Among 143 neuroblastomas, 115 tumors originated from the abdomen, 26 from extra-abdominal sites and 2 from unknown primary sites. Frequencies of stage 4 tumor and N-myc amplified tumor were lower in the extra-abdominal group than in the abdominal group (34.6% vs. 60.0%, P=0.019 and 4.2% vs. 45.0%, P<0.001, respectively). Levels of lactate dehydrogenase, ferritin and neuron-specific enolase were significantly lower in the extra-abdominal group than in the abdominal group. The probability of 5-yr EFS (+/-95% confidence interval) was higher in the extra-abdominal group than in the abdominal group (94.4+/-10.6% vs. 69.4+/-9.4%, P=0.026). Taken together, neuroblastomas originating from extra-abdominal sites might be associated with more favorable clinical and biological characteristics and a better outcome than neuroblastomas originating from abdomen.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Clinical Significance of Segmental Chromosomal Aberrations in Patients with Neuroblastoma: First Report in Korean Population
Hana Lim, Meong Hi Son, Ju Kyung Hyun, Hee Won Cho, Hee Young Ju, Ji Won Lee, Keon Hee Yoo, Ki Woong Sung, Hong Hoe Koo
J Korean Med Sci. 2020;35(14):e82. doi: 10.3346/jkms.2020.35.e82.
Reference
-
1. Evans AE, D'Angio GJ, Propert K, Anderson J, Hann HW. Prognostic factor in neuroblastoma. Cancer. 1987. 59:1853–1859.2. Coldman AJ, Fryer CJ, Elwood JM, Sonley MJ. Neuroblastoma: influence of age at diagnosis, stage, tumor site, and sex on prognosis. Cancer. 1980. 46:1896–1901.
Article3. Matthay KK, Perez C, Seeger RC, Brodeur GM, Shimada H, Atkinson JB, Black CT, Gerbing R, Haase GM, Stram DO, Swift P, Lukens JN. Successful treatment of stage III neuroblastoma based on prospective biologic staging: a Children's Cancer Group study. J Clin Oncol. 1998. 16:1256–1264.
Article4. Brodeur GM, Seeger RC, Schwab M, Varmus HE, Bishop JM. Amplification of N-myc in untreated human neuroblastomas correlates with advanced disease stage. Science. 1984. 224:1121–1124.5. Seeger RC, Brodeur GM, Sather H, Dalton A, Siegel SE, Wong KY, Hammond D. Association of multiple copies of the N-myc oncogene with rapid progression of neuroblastomas. N Engl J Med. 1985. 313:1111–1116.6. Look AT, Hayes FA, Shuster JJ, Douglass EC, Castleberry RP, Bowman LC, Smith EI, Brodeur GM. Clinical relevance of tumor cell ploidy and N-myc gene amplification in childhood neuroblastoma: a Pediatric Oncology Group study. J Clin Oncol. 1991. 9:581–591.7. Look AT, Hayes FA, Nitschke R, McWilliams NB, Green AA. Cellular DNA content as a predictor of response to chemotherapy in infants with unresectable neuroblastoma. N Engl J Med. 1984. 311:231–235.
Article8. Shimada H, Chatten J, Newton WA Jr, Sachs N, Hamoudi AB, Chiba T, Marsden HB, Misugi K. Histopathologic prognostic factors in neuroblastic tumors: definition of subtypes of ganglioneuroblastoma and an age-linked classification of neuroblastomas. J Natl Cancer Inst. 1984. 73:405–416.
Article9. Shimada H, Ambros IM, Dehner LP, Hata J, Joshi VV, Roald B, Stram DO, Gerbing RB, Lukens JN, Matthay KK, Castleberry RP. The International Neuroblastoma Pathology Classification (the Shimada system). Cancer. 1999. 86:364–372.
Article10. Joshi VV, Cantor AB, Brodeur GM, Look AT, Shuster JJ, Altshuler G, Larkin EW, Holbrook CT, Silverman JF, Norris HT. Correlation between morphologic and other prognostic markers of neuroblastoma. A study of histologic grade, DNA index, N-myc gene copy number, and lactic dehydrogenase in patients in the Pediatric Oncology Group. Cancer. 1993. 71:3173–3181.11. Shuster JJ, McWilliams NB, Castleberry R, Nitschke R, Smith EI, Altshuler G, Kun L, Brodeur G, Joshi V, Vietti T. Serum lactate dehydrogenase in childhood neuroblastoma. A Pediatric Oncology Group recursive partitioning study. Am J Clin Oncol. 1992. 15:295–303.
Article12. Hann HW, Evans AE, Siegel SE, Wong KY, Sather H, Dalton A, Hammond D, Seeger RC. Prognostic importance of serum ferritin in patients with Stages III and IV neuroblastoma: the Childrens Cancer Study Group experience. Cancer Res. 1985. 45:2843–2848.13. Zeltzer PM, Marangos PJ, Sather H, Evans A, Siegel S, Wong KY, Dalton A, Seeger RC, Hammond D. Prognostic importance of serum neuron specific enolase in local and widespread neuroblastoma. Prog Clin Biol Res. 1985. 175:319–329.14. Morris JA, Shochat SJ, Smith EI, Look AT, Brodeur GM, Cantor AB, Castleberry RP. Biological variables in thoracic neuroblastoma: a Pediatric Oncology Group study. J Pediatr Surg. 1995. 30:296–302.
Article15. Suita S, Tajiri T, Sera Y, Takamatsu H, Mizote H, Ohgami H, Kurosaki N, Hara T, Okamura J, Miyazaki S, Sugimoto T, Kawakami K, Tsuneyoshi M, Tasaka H, Yano H, Akiyama H, Ikeda K. The characteristics of mediastinal neuroblastoma. Eur J Pediatr Surg. 2000. 10:353–359.
Article16. Adams GA, Shochat SJ, Smith EI, Shuster JJ, Joshi VV, Altshuler G, Hayes FA, Nitschke R, McWilliams N, Castleberry RP. Thoracic neuroblastoma: a Pediatric Oncology Group study. J Pediatr Surg. 1993. 28:372–377.
Article17. Häberle B, Hero B, Berthold F, von Schweinitz D. Characteristics and outcome of thoracic neuroblastoma. Eur J Pediatr Surg. 2002. 12:145–150.
Article18. Horiuchi A, Muraji T, Tsugawa C, Nishijima E, Satho S, Takamizawa S, Misu H, Mabuchi O, Kanagawa K, Fujita M. Thoracic neuroblastoma: outcome of incomplete resection. Pediatr Surg Int. 2004. 20:714–718.
Article19. Cruccetti A, Kiely EM, Spitz L, Drake DP, Pritchard J, Pierro A. Pelvic neuroblastoma: low mortality and high morbidity. J Pediatr Surg. 2000. 35:724–728.
Article20. Moukheiber AK, Nicollas R, Roman S, Coze C, Triglia JM. Primary pediatric neuroblastic tumors of the neck. Int J Pediatr Otorhinolaryngol. 2001. 60:155–161.
Article21. Abramson SJ, Berdon WE, Ruzal-Shapiro C, Stolar C, Garvin J. Cervical neuroblastoma in eleven infants-a tumor with favorable prognosis. Clinical and radiologic (US, CT, MRI) findings. Pediatr Radiol. 1993. 23:253–257.22. Berdon WE, Stylianos S, Ruzal-Shapiro C, Hoffer F, Cohen M. Neuroblastoma arising from the organ of Zuckerkandl: an unusual site with a favorable biologic outcome. Pediatr Radiol. 1999. 29:497–502.
Article23. Brodeur GM, Pritchard J, Berthold F, Carlsen NL, Castel V, Castleberry RP, De Bernardi B, Evans AE, Favrot M, Hedborg F, Kaneto M, Kemshead J, Lampert F, Lee RE, Look AT, Pearson AD, Philip T, Roald B, Sawada T, Seeger RC, Tsuchida Y, Voute PA. Revisions of the international criteria for neuroblastoma diagnosis, staging, and response to treatment. J Clin Oncol. 1993. 11:1466–1477.
Article24. Sung KW, Lee SH, Yoo KH, Jung HL, Cho EJ, Koo HH, Lee SK, Kim J, Lim DH, Suh YL, Kim DW. Tandem high-dose chemotherapy and autologous stem cell rescue in patients over 1 year of age with stage 4 neuroblastoma. Bone Marrow Transplant. 2007. 40:37–45.
Article25. Matthay KK, Villablanca JG, Seeger RC, Stram DO, Harris RE, Ramsay NK, Swift P, Shimada H, Black CT, Brodeur GM, Gerbing RB, Reynolds CP. Children's Cancer Group. Treatment of high-risk neuroblastoma with intensive chemotherapy, radiotherapy, autologous bone marrow transplantation, and 13-cis-retinoic acid. N Engl J Med. 1999. 341:1165–1173.
Article26. Ladenstein R, Philip T, Lasset C, Hartmann O, Garaventa A, Pinkerton R, Michon J, Pritchard J, Klingebiel T, Kremens B, Pearson A, Coze C, Paolucci P, Frappaz D, Gadner H, Chauvin F. Multivariate analysis of risk factors in stage 4 neuroblastoma patients over the age of one year treated with megatherapy and stem-cell transplantation: a report from the European Bone Marrow Transplantation Solid Tumor Registry. J Clin Oncol. 1998. 16:953–965.
Article27. Berthold F, Boos J, Burdach S, Erttmann R, Henze G, Hermann J, Klingebiel T, Kremens B, Schilling FH, Schrappe M, Simon T, Hero B. Myeloablative megatherapy with autologous stem-cell rescue versus oral maintenance chemotherapy as consolidation treatment in patients with high-risk neuroblastoma: a randomized controlled trial. Lancet Oncol. 2005. 6:649–658.28. George RE, Li S, Medeiros-Nancarrow C, Neuberg D, Marcus K, Shamberger RC, Pulsipher M, Grupp SA, Diller L. High-risk neuroblastoma treated with tandem autologous peripheral-blood stem cellsupported transplantation: long-term survival update. J Clin Oncol. 2006. 24:2891–2896.
Article29. Kletzel M, Katzenstein HM, Haut PR, Yu AL, Morgan E, Reynolds M, Geissler G, Marymount MH, Liu D, Kalapurakal JA, Shore RM, Bardo DM, Schmoldt J, Rademaker AW, Cohn SL. Treatment of high-risk neuroblastoma with triple-tandem high-dose therapy and stem-cell rescue: results of the Chicago Pilot II Study. J Clin Oncol. 2002. 20:2284–2292.
Article