J Korean Med Sci.
2010 Mar;25(3):485-488. 10.3346/jkms.2010.25.3.485.
Balloon Valvuloplasty for Neonatal Critical Pulmonary Valvar Stenosis with IVC Interruption: Pitfalls of the Transumbilical Approach
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children's Hospital, Seoul, Korea. eunjbaek@snu.ac.kr
- KMID: 1778049
- DOI: http://doi.org/10.3346/jkms.2010.25.3.485
Abstract
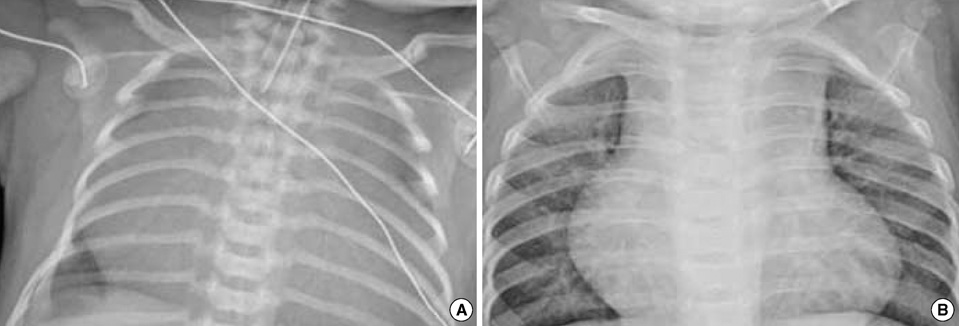
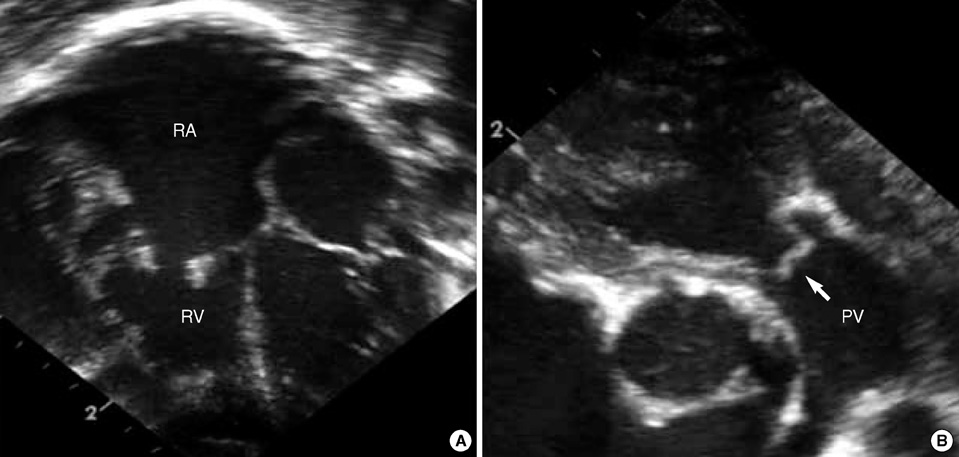
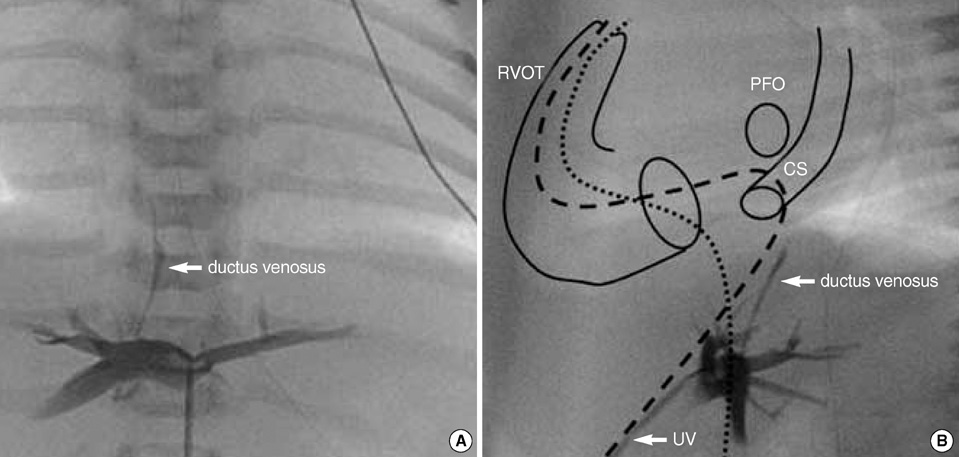
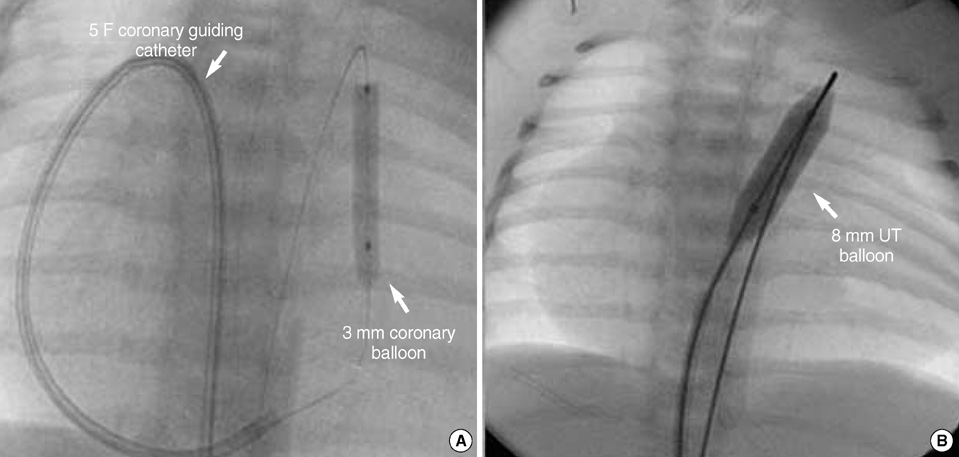
- Transcatheter balloon pulmonary valvuloplasty (BPV) is considered to be the treatment of choice for neonates with critical pulmonary valvar stenosis (PVS) or pulmonary valvar atresia with intact ventricular septum accompanied by reasonable right ventricular volume. The percutaneous femoral venous access is the most preferred route for BPV in most cardiac centers. We report herein the case of a newborn baby with critical PVS with inferior vena cava interruption, severe tricuspid regurgitation and a severely enlarged right atrium. We tried BPV through the transumbilical approach with difficulty, but he was successfully treated with the assistance of a coronary artery guiding catheter.
MeSH Terms
Figure
Reference
-
1. Kan JS, White RI Jr, Mitchell SE, Gardner TJ. Percutaneous balloon valvuloplasty: a new method for treating congenital pulmonary-valve stenosis. N Engl J Med. 1982. 30:540–542.
Article2. Weber HS. Initial and late results after catheter intervention for neonatal critical pulmonary valve stenosis and atresia with intact ventricular septum: a technique in continual evolution. Catheter Cardiovasc Interv. 2002. 56:394–399.
Article3. Shim D, Lloyd TR, Cho KJ, Moorehead CP, Beekman RH 3rd. Transhepatic cardiac catheterization in children. Evaluation of efficacy and safety. Circulation. 1995. 9:1526–1530.4. Chaara A, Zniber L, el Haitem N, Benomar M. Percutaneous balloon valvuloplasty via the right internal jugular vein for valvular pulmonic stenosis with severe right ventricular failure. Am Heart J. 1989. 117:684–685.
Article5. Meyer WW, Lind J. The ductus venosus and the mechanism of its closure. Arch Dis Child. 1966. 41:597–605.
Article6. Linde LM, Higashino SM, Berman G, Sapin SO, Emmanouilides GC. Umbilical vessel cardiac catheterization and angiocardiography. Circulation. 1966. 34:984–988.
Article7. Abinader E, Zeltzer M, Riss E. Transumbilical atrial septostomy in the newborn. Am J Dis Child. 1970. 119:354–355.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous transluminal balloon valvuloplasty for congenital pulmonary valvular stenosis
- Percutaneous transluminal balloon valvuloplasty for congenital pulmonary valve stenosis and aortic valve stenosis
- Percutaneous Transluminal Balloon Valvuloplasty for Congenital Pulmonary Valve Stenosis
- Percutaneous Balloon Valvuloplasty with Trefoil Balloon Catheter for the Treatment of Congenital Pulmonary Stenosis in Children
- A Case of Balloon Valvuloplasty using Three Balloon Catheters in a Child with Pulmonic Stenosis