J Korean Med Sci.
2013 Nov;28(11):1627-1631. 10.3346/jkms.2013.28.11.1627.
Risk Factors for Long-term Outcomes after Initial Treatment in Hepatolithiasis
- Affiliations
-
- 1Digestive Disease Center, Department of Internal Medicine, Inha University School of Medicine, Incheon, Korea. inos@inha.ac.kr
- 2The National Center of Efficacy Evaluation for the Development of Health Products Targeting Digestive Disorders (NCEED), Incheon, Korea.
- 3Utah-Inha DDS & Advanced Therapeutics Research Center, Incheon, Korea.
- 4Department of Occupational and Environmental Medicine, Inha University School of Medicine, Incheon, Korea.
- KMID: 1777660
- DOI: http://doi.org/10.3346/jkms.2013.28.11.1627
Abstract
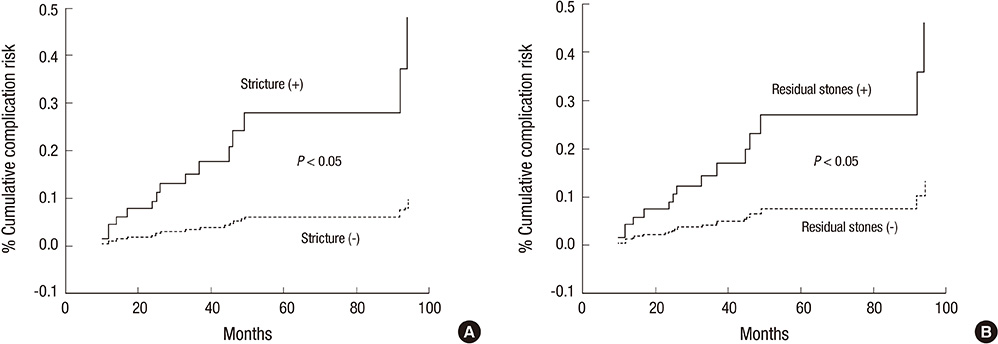
- Hepatobiliary complications, such as stone recurrence, recurrent cholangitis, liver abscess, secondary biliary cirrhosis, and cholangiocarcinoma may occur after treatment for hepatolithiasis. However, few previous studies have addressed the risk factors and long-term outcomes after initial treatment. Eighty-five patients with newly diagnosed hepatolithiasis, actively treated for hepatolithiasis, constituted the cohort of this retrospective study. Patients were treated by hepatectomy or nonoperative percutaneous transhepatic cholangioscopic lithotomy. Long-term complications, such as recurrent cholangitis, liver abscess, secondary biliary cirrhosis, and cholangiocarcinoma, and their relationships with clinical parameters were analyzed. The mean follow-up period was 57.4 months. The overall hepatobiliary complication rate after the treatment was 17.6%. Multivariate analysis of suspected risk factors showed that complications were associated with age (HR, 1.046; CI, 1.006-1.089), bile duct stricture (HR, 4.894; CI, 1.295-18.495), and residual stones (HR, 3.482; CI, 1.214-9.981). In conclusion, several long-term hepatobiliary complications occur after hepatolithiasis treatment, and regular observation is necessary in patients with concomitant biliary stricture or residual stones.
Keyword
MeSH Terms
Figure
Reference
-
1. Lee JY, Kim JS, Moon JM, Lim SA, Chung W, Lim EH, Lee BJ, Park JJ, Bak YT. Incidence of cholangiocarcinoma with or without previous resection of liver for hepatolithiasis. Gut Liver. 2013; 7:475–479.2. Uchiyama K, Kawai M, Ueno M, Ozawa S, Tani M, Yamaue H. Reducing residual and recurrent stones by hepatectomy for hepatolithiasis. J Gastrointest Surg. 2007; 11:626–630.3. Oh HC, Lee SK, Lee TY, Kwon S, Lee SS, Seo DW, Kim MH. Analysis of percutaneous transhepatic cholangioscopy-related complications and the risk factors for those complications. Endoscopy. 2007; 39:731–736.4. Hwang JH, Yoon YB, Kim YT, Cheon JH, Jeong JB. Risk factors for recurrent cholangitis after initial hepatolithiasis treatment. J Clin Gastroenterol. 2004; 38:364–367.5. Sakpal SV, Babel N, Chamberlain RS. Surgical management of hepatolithiasis. HPB (Oxford). 2009; 11:194–202.6. Kim EH, Kim HJ, Oh HC, Lee KH, Jung JY, Kim S, Lee SS, Seo DW, Kim MH, Lee SK. The usefulness of percutaneous transhepatic cholangioscopy for identifying malignancies in distal common bile duct strictures. J Korean Med Sci. 2008; 23:579–585.7. Yang SH, Lee SE, Jang JY, Ryu JK, Kim YT, Yun YB, Kim SW. Clinical and epidemiological analysis of gallstone patients: focused on 25-year experience of surgically treated patients. Korean J Gastroenterol. 2007; 50:42–50.8. Tian J, Li JW, Chen J, Fan YD, Bie P, Wang SG, Zheng SG. Laparoscopic hepatectomy with bile duct exploration for the treatment of hepatolithiasis: an experience of 116 cases. Dig Liver Dis. 2013; 45:493–498.9. Kim MH, Lee SS. Current status of intrahepatic stones in Korea. Korean J Gastroenterol. 2003; 42:89–95.10. Kim BW, Wang HJ, Kim WH, Kim MW. Favorable outcomes of hilar duct oriented hepatic resection for high grade Tsunoda type hepatolithiasis. World J Gastroenterol. 2006; 12:431–436.11. Cheon YK, Cho YD, Moon JH, Lee JS, Shim CS. Evaluation of long-term results and recurrent factors after operative and nonoperative treatment for hepatolithiasis. Surgery. 2009; 146:843–853.12. Lee SE, Jang JY, Lee JM, Kim SW. Selection of appropriate liver resection in left hepatolithiasis based on anatomic and clinical study. World J Surg. 2008; 32:413–418.13. Eun JR, Jang BI, Lee JY, Kim KO, Lee SH, Kim TN, Lee HJ. Clinical characteristics of intrahepatic cholangiocarcinoma and prognostic factors in patients who received non-surgical treatment. Korean J Gastroenterol. 2009; 54:227–234.14. Lai EC, Ngai TC, Yang GP, Li MK. Laparoscopic approach of surgical treatment for primary hepatolithiasis: a cohort study. Am J Surg. 2010; 199:716–721.15. Chen C, Huang M, Yang J, Yang C, Yeh Y, Wu H, Chou D, Yueh S, Nien C. Reappraisal of percutaneous transhepatic cholangioscopic lithotomy for primary hepatolithiasis. Surg Endosc. 2005; 19:505–509.16. Catena M, Aldrighetti L, Finazzi R, Arzu G, Arru M, Pulitanò C, Ferla G. Treatment of non-endemic hepatolithiasis in a Western country: the role of hepatic resection. Ann R Coll Surg Engl. 2006; 88:383–389.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk Factors for Cholangiocarcinomas Associated with Hepatolithiasis
- Development of perihilar cholangiocarcinoma at 29 years after first hepatectomy for hepatolithiasis
- Recent Treatment Modalities for Hepatolithiasis and Long-term Outcomes
- Analysis of the Risk Factors for Cholangitis Occurring after Treatment of Hepatolithiasis
- Three Cases of Unresectable Cholangiocarcinoma Diagnosed after Removal of Hepatolithiasis by Percutaneous Transhepatic Cholangioscopy