Korean J Radiol.
2005 Dec;6(4):248-255. 10.3348/kjr.2005.6.4.248.
Prospective Comparison of Collagen Plug (Angio-SealTM) and Suture-Mediated (the Closer STM) Closure Devices at Femoral Access Sites
- Affiliations
-
- 1Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Korea. hgroh@kuh.ac.kr
- 2Department of Radiology, Konkuk University Hospital, Korea.
- KMID: 1777283
- DOI: http://doi.org/10.3348/kjr.2005.6.4.248
Abstract
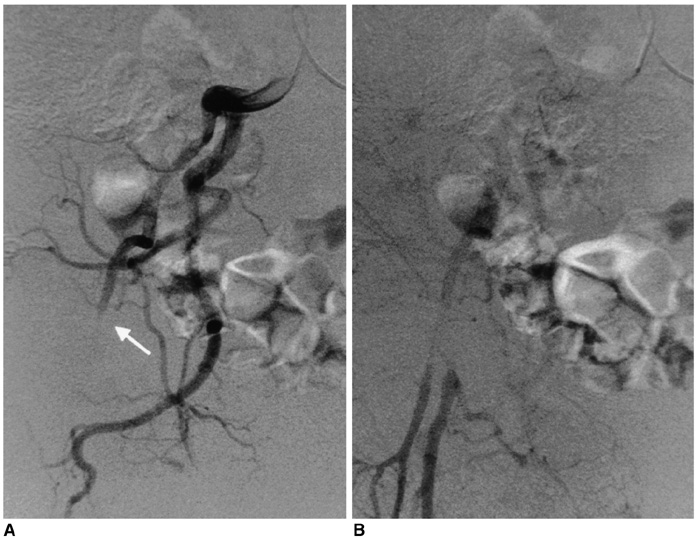
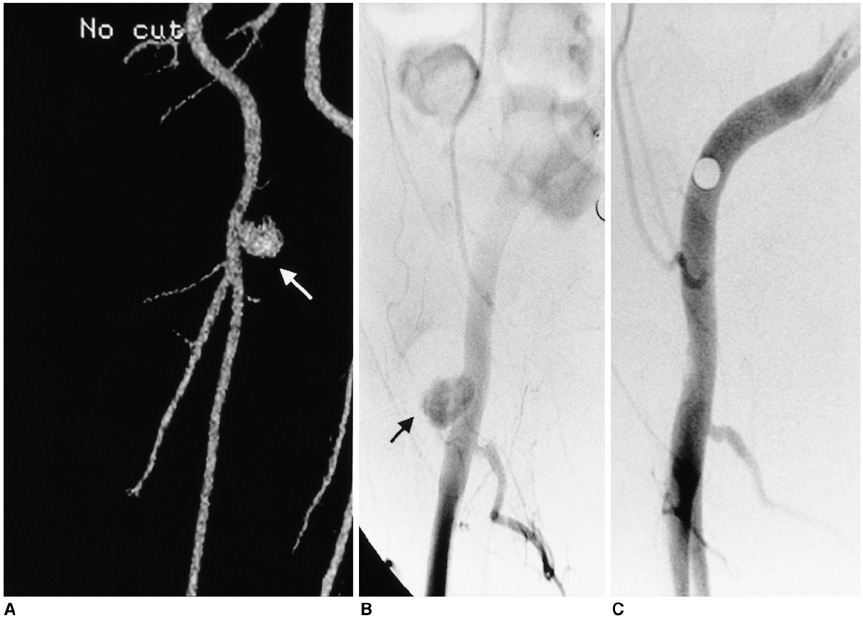
OBJECTIVE
Rapid and effective hemostasis at femoral puncture sites minimizes both the hospital stay and patient discomfort. Therefore, a variety of arterial closure devices have been developed to facilitate the closure of femoral arteriotomy. The objective of this prospective study was to compare the efficacy of two different closure devices; a collagen plug device (Angio-Seal) and a suture-mediated closure device (the Closer S). MATERIALS AND METHODS: From March 28, 2003 to August 31, 2004, we conducted a prospective study in which 1, 676 cases of 1, 180 patients were treated with two different types of closure device. Angio-Seal was used in 961 cases and the Closer S in 715 cases. The efficacy of the closure devices was assessed, as well as complications occurring at the puncture sites. RESULTS: Successful immediate hemostasis was achieved in 95.2% of the cases treated with Angio-Seal, and in 89.5% of the cases treated with the Closer S (p < 0.05). The rates of minor and major complications occurring between the two groups were not significantly different. In the Closer S group, we observed four major complications (0.6%), that consisted of one massive retroperitoneal hemorrhage (surgically explored) and three pseudoaneurysms. In the Angio-Seal group, we observed three major complications (0.3%) that consisted of one femoral artery occlusion, one case of infection treated with intravenous antibiotics and one pseudoaneurysm. CONCLUSION: The use of Angio-Seal was found to be more effective than that of the Closer S with regard to the immediate hemostasis of the femoral puncture sites. However, we detected no significant differences in the rate at which complications occurred.
Keyword
MeSH Terms
Figure
Reference
-
1. Kussmaul WG III, Buchibinder M, Whitlow PL, Aker UT, Heuser RR, King SB, et al. Rapid arterial hemostasis and decreased access site complications after cardiac catheterization and angioplasty: results of randomized trial of novel hemostatic device. J Am Coll Cardiol. 1995. 26:1685–1692.2. Sanborn TA, Gibbs HH, Brinker JA, Knopf WD, Kosinski EJ, Roubin GS. A multicenter randomized trial comparing a percutaneous collagen hemostasis device with conventional manual compression after diagnostic angiography and angioplasty. J Am Coll Cardiol. 1993. 22:1273–1279.3. Cremonesi A, Castriota F, Tarantino F, Troiani E, Ricci E, El Jamal B, et al. Femoral arterial hemostasis using the Angio-Seal system after coronary and vascular percutaneous angioplasty and stenting. J Invas Cardiol. 1998. 10:464–469.4. Kapadia SR, Raymond R, Knopf W, Jenkins S, Chapekis A, Ansel G, et al. The 6 Fr Angio-Seal arterial closure devise: results from a multicenter prospective registry. J Am Cardiol. 2001. 87:789–791.5. Silber S, Bjorvik A, Muhling H, Rosch A. Usefulness of collagen plugging with VasoSeal after PTCA as compared to manual compression with identical sheath dwell times. Cathet Cardiovasc Diagn. 1998. 43:421–427.6. Schrader R, Steinbacher S, Burger W, Kadel C, Vallbracht C, Kaltenbach M. Collagen application for sealing of arterial puncture sites in comparison to pressure dressing: a randomized trial. Cathet Cardiovasc Diagn. 1992. 27:298–302.7. Carere RG, Webb JG, Ahmed T, Dodeck AA. Initial experience using Prostar: a new device for percutaneous suture-mediated closure of arterial puncture sites. Cathet Cardiovasc Diagn. 1996. 37:367–372.8. Chamberlin JR, Lardi AB, McKeever LS, Wang MH, Ramadurai G, Grunenwald P, et al. Use of vascular sealing device (VasoSeal and Perclose) versus assisted manual compression (Femostop) in transcatheter coronary interventions requiring abciximab (ReoPro). Cathet Cardiovasc Intervent. 1999. 47:143–147.9. Gerckens U, Cattelaens N, Lampe EG, Grube E. Management of arterial puncture site after catheterization procedures: evaluating a suture-mediated closure device. Am J Cardiol. 1998. 83:1658–1663.10. Shrake KL. Comparison of major complication rates associated with four methods of arterial closure. Am J Cardiol. 2000. 85:1024–1025.11. Baim DS, Knopf WD, Hinohara T, Schwarten DE, Schatz RA, Pinkerton CA, et al. Suture-mediated closure of the femoral access site after cardiac catheterizations: results of the Suture to Ambulate and Discharge (STAND I and STAND II) trials. Am J Cardiol. 2000. 85:864–869.12. Sievert H, Wander T, Mussing S, Bolscher S. The Perclose device for hemostasis after antegrade puncture of the femoral artery: a randomized trial. Am J Cardiol. 1998. 82:Suppl 7A. 34S–35S.13. Popma JJ, Satler LF, Pichard AD, Kent KM, Campbell A, Chuang YC, et al. Vascular complications after balloon and new device angioplasty. Circulation. 1993. 88(pt 1):1569–1578.14. Muller DW, Shamir KJ, Ellis SG, Topol EJ. Peripheral vascular complications after conventional and complex percutaneous coronary interventional procedures. Am J Cardiol. 1992. 69:63–68.15. Waksman R, King SB, Douglas JS, Shen Y, Ewing H, Mueller L, et al. Predictors of groin complications after balloon and new device coronary intervention. Am J Cardiol. 1995. 75:886–889.16. Oweida SW, Roubin GS, Smith RB, Salam AA. Postcatheterization vascular complications associated with percutaneous transluminal coronary angioplasty. J Vasc Surg. 1990. 12:310–315.17. Skillman JJ, Ducksoo K, Baim DS. Vascular complications of percutaneous femoral cardiac interventions: incidence and operative repair. Arch Surg. 1988. 123:1207–1212.18. Babu SC, Piccorelli GO, Shah PM, Stein JH, Clauss RH. Incidence and results of arterial complications among 16,350 patients undergoing cardiac catheterization. J Vasc Surg. 1989. 10:113–116.19. Kaufmann J, Moglia R, Lacy C, Dinerstein C, Moreyra A. Peripheral vascular complications from percutaneous transluminal coronary angioplasty: a comparison with transfemoral cardiac catheterization. Am J Med Sci. 1989. 297:22–25.20. EPIC Investigators. Use of a monoclonal antibody directed against the platelet glycoprotein IIb/IIIa receptor in high-risk coronary angioplasty. N Engl J Med. 1994. 330:956–961.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of Femoral Vascular Closure Devices in Patients Treated with Anticoagulant, Abciximab or Thrombolytics during Percutaneous Endovascular Procedures
- Intraluminal Snared-Atheroma Causing Common Femoral Artery Stenosis after Using Perclose Suture-Mediated Closure System
- Ultrasonographic features of vascular closure devices: initial and 6-month follow-up results
- Surgical Treatment of Femoral & Popliteal Arteries Thrombosis Caused by Collagen Material Closure Device: A case report
- Efficacy and Complications of Angio-Seal(r) Device in Patients Undergoing Coronary Angiography and Angioplasty