Korean J Radiol.
2009 Aug;10(4):398-401. 10.3348/kjr.2009.10.4.398.
Myopericytoma Involving the Parotid Gland as Depicted on Multidetector CT
- Affiliations
-
- 1Department of Radiology, West China Hospital, Sichuan University, Sichuan 610041, China. cjr.yujianqun@vip.163.com
- 2Department of Pathology, West China College of Stomatology, Sichuan University, Sichuan 610041, China.
- KMID: 1777269
- DOI: http://doi.org/10.3348/kjr.2009.10.4.398
Abstract
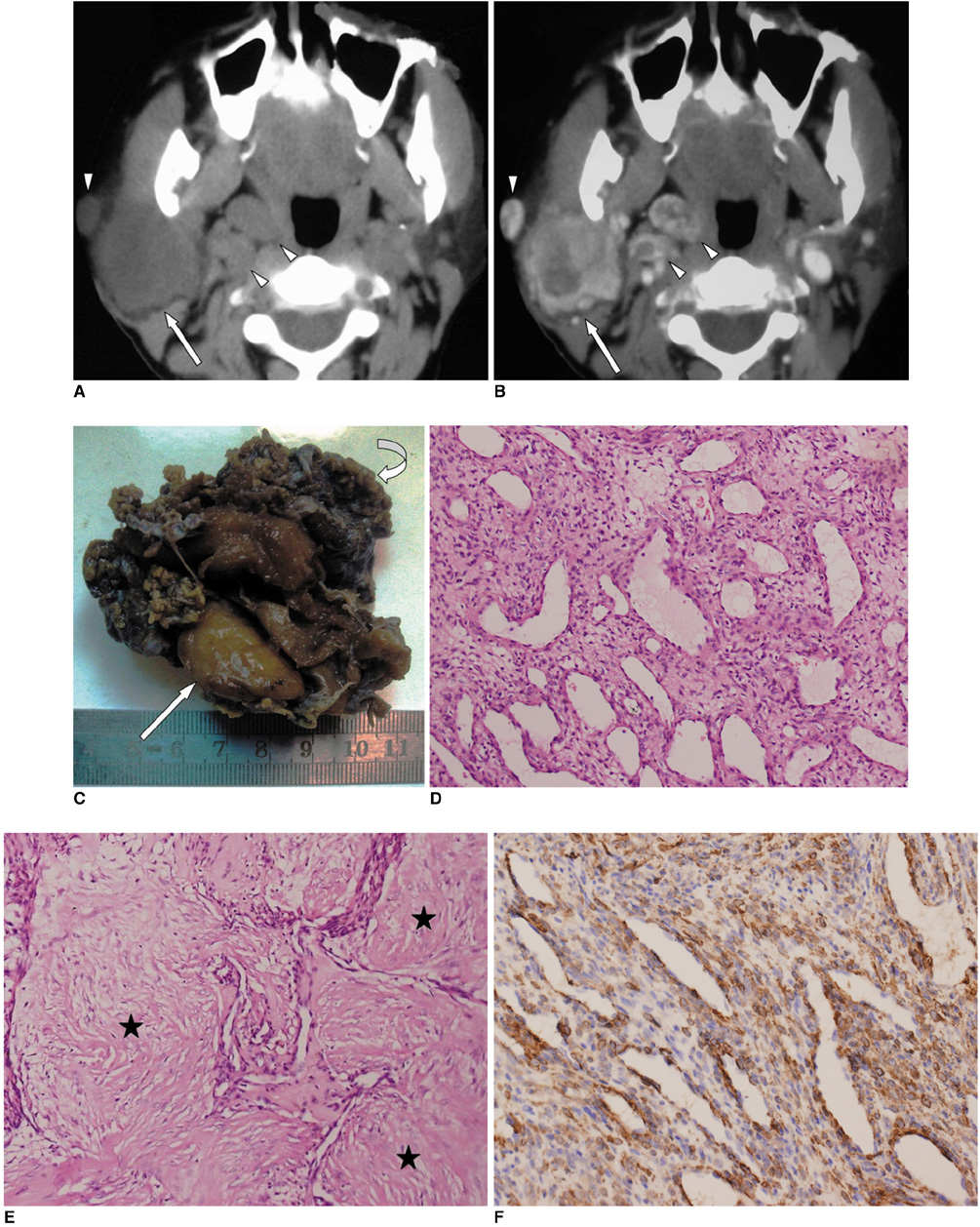
- Myopericytoma is a newly proposed subgroup of perivascular tumors in the World Health Organization classification of soft tissue tumors. In this study, we report a case of a benign myopericytoma with detailed multidetector CT (MDCT) findings in the parotid gland, a location that has not been described for this type of tumor previously. The clinical presentation, imaging features, histopathological and immunohistochemical findings, and the differential diagnosis with other tumors in the parotid gland are described and reviewed.
Keyword
MeSH Terms
Figure
Reference
-
1. McMenamin ME, Fletcher CD. Malignant myopericytoma: expanding the spectrum of tumours with myopericytic differentiation. Histopathology. 2002. 41:450–460.2. Mentzel T, Dei Tos AP, Sapi Z, Kutzner H. Myopericytoma of skin and soft tissues: clinicopathologic and immunohistochemical study of 54 cases. Am J Surg Pathol. 2006. 30:104–113.3. McMenamin ME. Fletcher CD, Unni KK, Merteus F, editors. Myopericytoma. Pathology and genetics of tumors of soft tissue and bone. WHO classification of tumors. 2002. Lyon: IARC Press;138–139.4. Requena L, Kutzner H, Hugel H, Rutten A, Furio V. Cutaneous adult myofibroma: a vascular neoplasm. J Cutan Pathol. 1996. 23:445–457.5. Granter SR, Badizadegan K, Fletcher CD. Myofibromatosis in adults, glomangiopericytoma, and myopericytoma: a spectrum of tumors showing perivascular myoid differentiation. Am J Surg Pathol. 1998. 22:513–525.6. Cox DP, Giltman L. Myopericytoma of the thoracic spine: a case report. Spine. 2003. 28:E30–E32.7. Rousseau A, Kujas M, van Effenterre R, Boch AL, Carpentier A, Leroy JP. Primary intracranial myopericytoma: report of three cases and review of the literature. Neuropathol Appl Neurobiol. 2005. 31:641–648.8. Wilson T, Hellquist HB, Ray S, Pickles J. Intranasal myopericytoma. A tumour with perivascular myoid differentiation: the changing nomenclature for haemangiopericytoma. J Laryngol Otol. 2007. 121:786–789.9. McMenamin ME, Calonje E. Intravascular myopericytoma. J Cutan Pathol. 2002. 29:557–561.10. Datta V, Rawal YB, Mincer HH, Anderson MK. Myopericytoma of the oral cavity. Head Neck. 2007. 29:605–608.11. Harish S, O'Donnell P, Briggs TW, Saifuddin A, Flanagan AM. Myopericytoma in Kager's fat pad. Skeletal Radiol. 2007. 36:165–169.12. Oktem F, Karaman E, Mamak A, Yilmaz S, Erdamar S. Hemangiopericytoma of the parotid gland: a case report. Kulak Burun Bogaz Ihtis Derg. 2007. 17:112–115.13. Mortele B, Lemmerling M, Seynaeve P, Clarysse P, Quintens F, Kunnen M. Hemangiopericytoma of the parotid gland: CT and MR features. Eur Radiol. 2001. 11:1073–1075.14. Takeishi M, Makino Y, Nishioka H, Miyawaki T, Kurihara K. Kimura disease: diagnostic imaging findings and surgical treatment. J Craniofac Surg. 2007. 18:1062–1067.15. Kim HJ, Lee HK, Seo JJ, Kim HJ, Shin JH, Jeong AK, et al. MR imaging of solitary fibrous tumors in the head and neck. Korean J Radiol. 2005. 6:136–142.16. Guerra MFM, Amat CG, Campo FR, Perez JS. Solitary fibrous tumor of the parotid gland: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002. 94:78–82.17. Yerli H, Aydin E, Coskun M, Geyik E, Ozluoglu LN, Haberal N, et al. Dynamic multislice computed tomography findings for parotid gland tumors. J Comput Assist Tomogr. 2007. 31:309–316.18. Choi DS, Na DG, Byun HS, Ko YH, Kim CK, Cho JM, et al. Salivary gland tumors: evaluation with two-phase helical CT. Radiology. 2000. 214:231–236.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple Myopericytoma of the Face and Parotid Gland
- Unilateral Agenesis of the Parotid Gland: A Case Report
- Age-dependent difference in the computed tomography numbers of the normal parotid gland of Koreans
- Extramedullary Relapse of Acute Lymphoblastic Leukemia Involving the Parotid Gland: A Case Report and Literature Review
- A Case of Parotid Tuberculosis Mimicking Benign Tumor of Parotid Gland