Korean J Gastroenterol.
2009 Aug;54(2):130-134. 10.4166/kjg.2009.54.2.130.
Cerebral Lipiodol Embolism after Transcatheter Arterial Chemoembolization of Hepatocellular Carcinoma
- Affiliations
-
- 1Miraero 21 Medical Center, Gwangju, Korea.
- 2Department of Internal Medicine, Chonnam National University Medical School, Gwangju, Korea. choisk@chonnam.ac.kr
- KMID: 1775969
- DOI: http://doi.org/10.4166/kjg.2009.54.2.130
Abstract
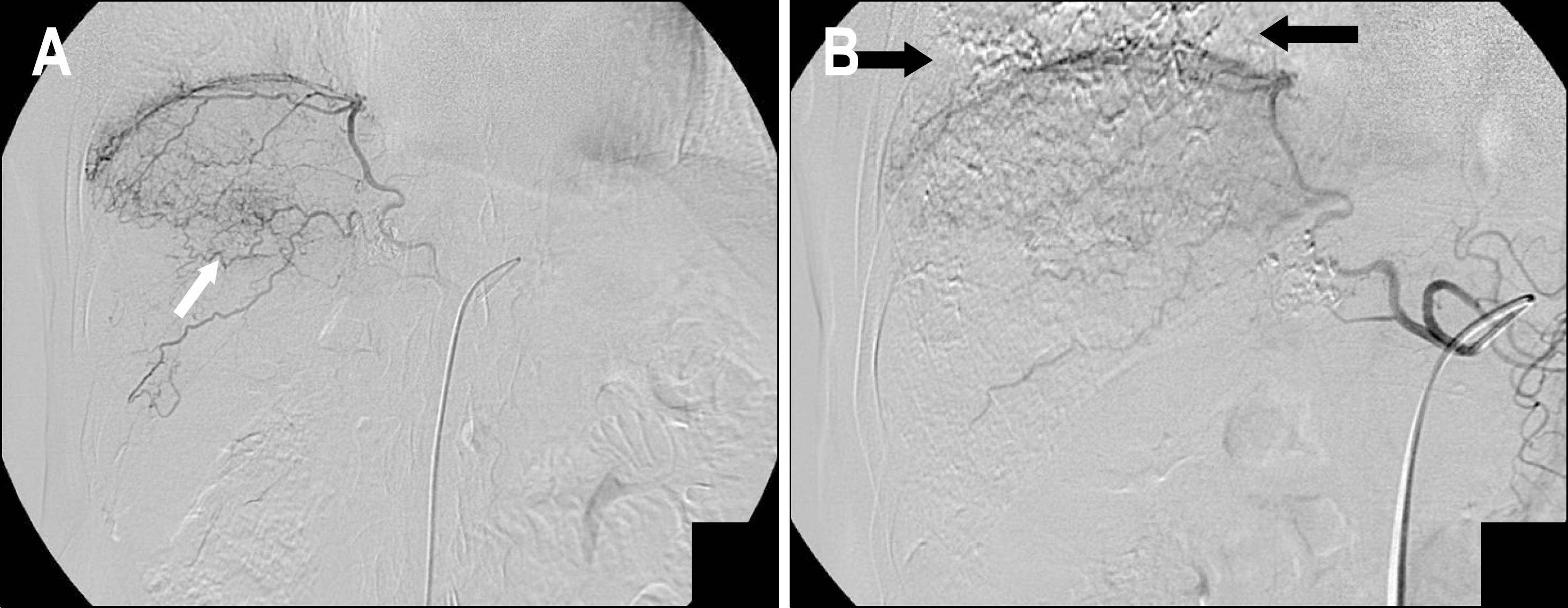
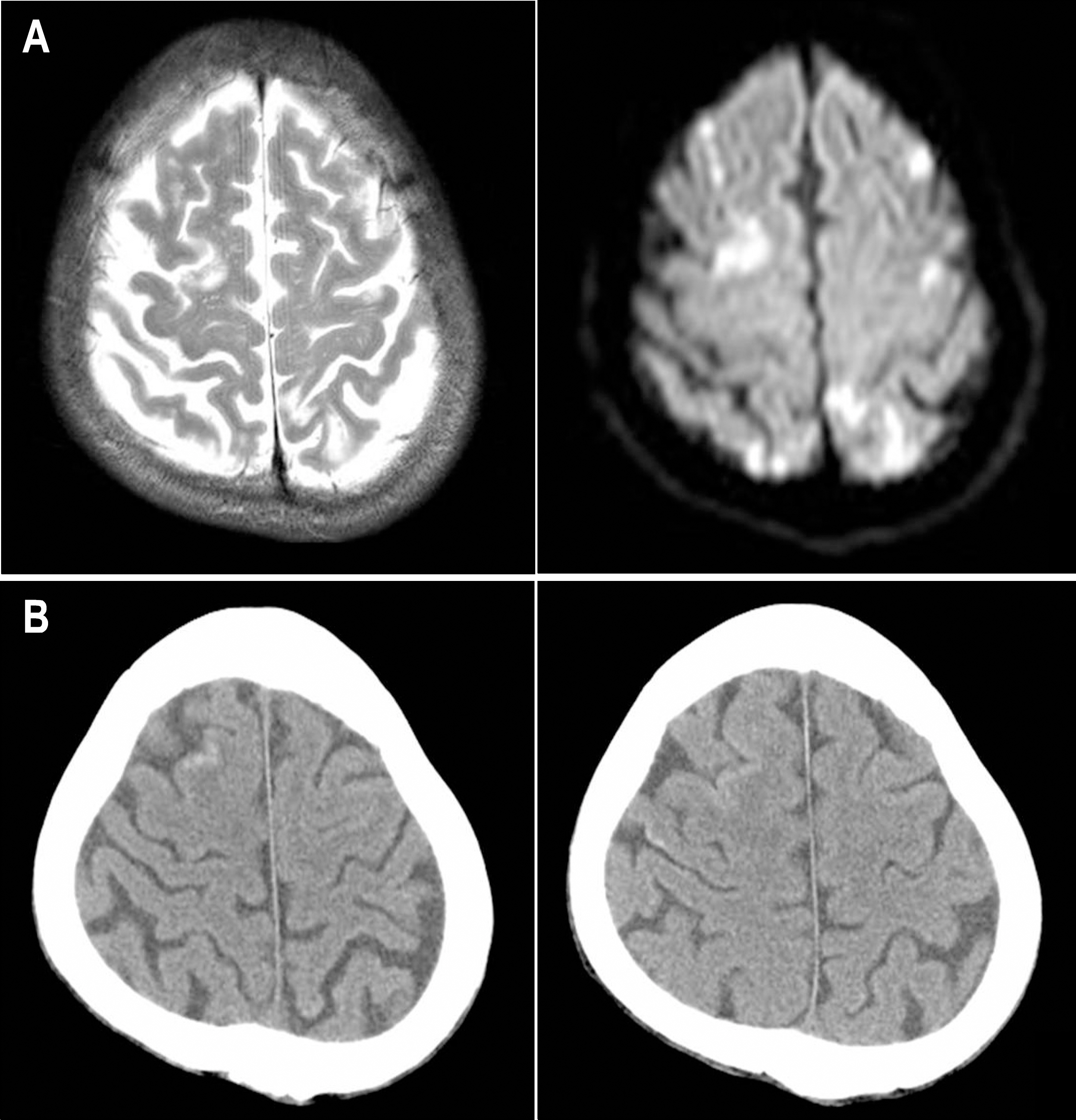
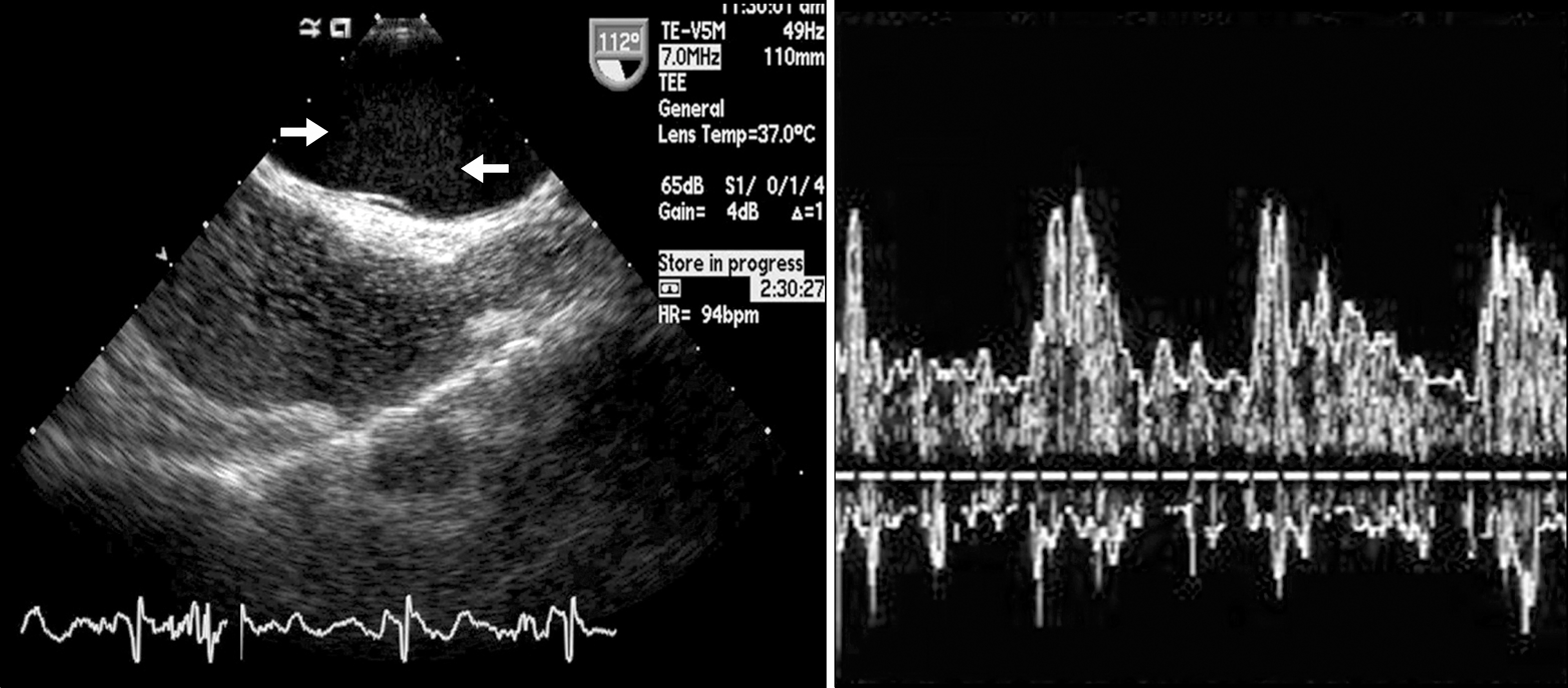
- Transcatheter arterial chemoembolization (TACE) is the mainstay of treatment for unresectable hepatocellular carcinoma (HCC). Although various complications of TACE have been reported, cerebral lipiodol embolism after TACE is rare. We report a 67-year-old man, who had patent foramen ovale and developed cerebral lipiodol embolism after TACE via the inferior phrenic artery. At 20 months after third TACE of 3 cm sized HCC in the left hepatic lobe, computed tomography (CT) revealed about 1.6 cm newly developed HCC in the anterior superior segment of right hepatic lobe. The angiogram revealed the HCC was supplied from the right inferior phrenic artery. Toward the end of TACE, there were accumulations of the iodized oil in the pulmonary vasculature. Immediately after TACE, he complained of weakness in right upper and lower limbs and sensory decrease in right limbs and right hemitrunk. Magnetic resonance imaging revealed a cerebral lipiodol embolism. Transesophageal echocardiography revealed no visible thrombi but contrast-echocardiography using hand agitated saline revealed an intracardiac right to left shunt consistent with patent foramen ovale. Motor weakness and sensory decrease were gradually improved, and all neurological symptoms disappeared over 4 weeks.
MeSH Terms
-
Aged
Carcinoma, Hepatocellular/complications/diagnosis/*therapy
*Chemoembolization, Therapeutic
Contrast Media/*adverse effects/diagnostic use
Humans
Intracranial Embolism/*diagnosis/*etiology/ultrasonography
Iodized Oil/*adverse effects/diagnostic use
Liver Neoplasms/complications/diagnosis/*therapy
Magnetic Resonance Imaging
Male
Tomography, X-Ray Computed
Figure
Reference
-
1. Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma. Lancet. 2003; 362:1907–1917.
Article2. Chen MS, Li JQ, Zhang YQ, et al. High-dose iodized oil transcatheter arterial chemoembolization for patients with large hepatocellular carcinoma. World J Gastroenterol. 2002; 8:74–78.
Article3. Tang ZY. Hepatocellular carcinoma–cause, treatment and metastasis. World J Gastroenterol. 2001; 7:445–454.
Article4. Yip D, Findlay M, Boyer M, Tattersall MH. Hepatocellular carcinoma in central Sydney: a 10-year review of patients seen in a medical oncology department. World J Gastroenterol. 1999; 5:483–487.5. Ramsey DE, Kernagis LY, Soulen MC, Geschwind JF. Chemoembolization of hepatocellular carcinoma. J Vasc Interv Radiol. 2002; 13(suppl):S211–S221.
Article6. Sakamoto I, Aso N, Nagaoki K, et al. Complications associated with transcatheter arterial embolization for hepatic tumors. Radiographics. 1998; 18:605–619.
Article7. Wu RH, Tzeng WS, Chang CM. Iodized oil embolization to brain following transcatheter arterial embolization of liver. J Gastroenterol Hepatol. 2005; 20:1465–1467.
Article8. Yoo KM, Yoo BG, Kim KS, Lee SU, Han BH. Cerebral lipiodol embolism during transcatheter arterial chemoembolization. Neurology. 2004; 63:181–183.
Article9. Takao H, Makita K, Doi I, Watanabe T. Cerebral lipiodol embolism after transcatheter arterial chemoembolization of hepatocellular carcinoma. J Comput Assist Tomogr. 2005; 29:680–682.
Article10. Tajima T, Honda H, Kuroiwa T, et al. Pulmonary complications after hepatic artery chemoembolization or infusion via the inferior phrenic artery for primary liver cancer. J Vasc Interv Radiol. 2002; 13:893–900.
Article11. Cho SH, Kim JH, Kim BS, Jang J. A case of acute lung injury complicated by transcatheter arterial chemoembolization for hepatocellular carcinoma. Tuberc Respir Dis. 1995; 42:781–786.
Article12. Chung JW, Park JH, Im JG, Han JK, Han MC. Pulmonary oil embolism after transcatheter oily chemoembolization of hepatocellular carcinoma. Radiology. 1993; 187:689–693.
Article13. Kan Z, Sato M, Ivancev K, et al. Distribution and effect of iodized poppyseed oil in the liver after hepatic artery embolization: experimental study in several animal species. Radiology. 1993; 186:861–866.
Article14. Matsumoto K, Nojiri J, Takase Y, et al. Cerebral lipiodol embolism: a complication of transcatheter arterial chemoembolization for hepatocellular carcinoma. Cardiovasc Intervent Radiol. 2007; 30:512–514.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Fatal Case of Pulmonary Embolism after Transcatheter Arterial Chemoembolization for Hepatocellular Carcinoma
- Pulmonary Lipiodol Embolism after Transcatheter Chemoembolization for Hepatocellular Carcinoma
- The Suppression Effect of the Intrahepatic Recurrence of Transcatheter Arterial Chemoembolization with Cisplatin in the Hepatocellular Carcinoma Patients: The Comparison of Adriamycin-Lipiodol Emulsion Infusions with Adriamycin-Lipiodol Emulsion Infusions
- Massive Tumor Pulmonary Embolism Following Transcatheter Arterial Chemoembolization of Hepatocellular Carcinoma
- Lipiodol brain embolism through right inferior phrenic artery-pulmonary vein shunt after transcatheter arterial chemoembolization