J Korean Med Sci.
2014 Apr;29(4):581-586. 10.3346/jkms.2014.29.4.581.
The Timing of Surgical Ligation for Patent Ductus Arteriosus Is Associated with Neonatal Morbidity in Extremely Preterm Infants Born at 23-25 Weeks of Gestation
- Affiliations
-
- 1Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University, School of Medicine, Seoul, Korea. wonspark@skku.edu
- KMID: 1774466
- DOI: http://doi.org/10.3346/jkms.2014.29.4.581
Abstract
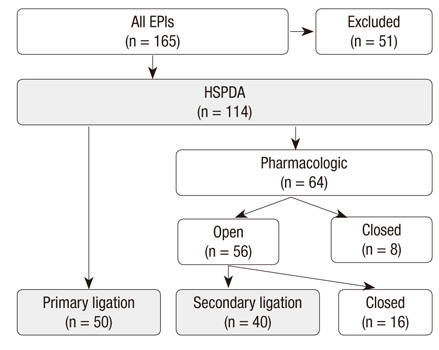
- The purpose of this study was to evaluate prognostic factors associated with surgical ligation for patent ductus arteriosus (PDA) in extremely preterm infants born at the limits of viability. Ninety infants who were born at 23-25 weeks of gestation and who received surgical ligation were included and their cases were retrospectively reviewed. Infants were classified into two different groups: survivors with no major morbidity (N), and non-survivors or survivors with any major morbidity (M). Clinical characteristics were compared between the groups. Possible prognostic factors were derived from this comparison and further tested by logistic regression analysis. The mean gestational age and the mean birth weight of M were significantly lower than those of N. Notably, the mean postnatal age at time of ligation in N was significantly later than that of the other group (17+/-12 vs 11+/-8 days in N and M, respectively). An adjusted analysis showed that delayed ligation (>2 weeks) was uniquely associated with a significantly decreased risk for mortality or composite morbidity after surgical ligation (OR, 0.105; 95% CI, 0.012-0.928). In conclusion, delayed surgical ligation for PDA (>2 weeks) is associated with decreased mortality or morbidities in extremely preterm infants born at 23-25 weeks of gestation.
Keyword
MeSH Terms
Figure
Reference
-
1. Koch J, Hensley G, Roy L, Brown S, Ramaciotti C, Rosenfeld CR. Prevalence of spontaneous closure of the ductus arteriosus in neonates at a birth weight of 1000 grams or less. Pediatrics. 2006; 117:1113–1121.2. Alexander F, Chiu L, Kroh M, Hammel J, Moore J. Analysis of outcome in 298 extremely low-birth-weight infants with patent ductus arteriosus. J Pediatr Surg. 2009; 44:112–117.3. Jhaveri N, Moon-Grady A, Clyman RI. Early surgical ligation versus a conservative approach for management of patent ductus arteriosus that fails to close after indomethacin treatment. J Pediatr. 2010; 157:381–387. 387.e14. McNamara PJ, Sehgal A. Towards rational management of the patent ductus arteriosus: the need for disease staging. Arch Dis Child Fetal Neonatal Ed. 2007; 92:F424–F427.5. Burstein J, Papile LA, Burstein R. Intraventricular hemorrhage and hydrocephalus in premature newborns: a prospective study with CT. AJR Am J Roentgenol. 1979; 132:631–635.6. Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, Wrage LA, Poole K. National Institutes of Child Health and Human Development Neonatal Research Network. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005; 116:1353–1360.7. Walsh MC, Kliegman RM, Fanaroff AA. Necrotizing enterocolitis: a practitioner's perspective. Pediatr Rev. 1988; 9:219–226.8. Malviya MN, Ohlsson A, Shah SS. Surgical versus medical treatment with cyclooxygenase inhibitors for symptomatic patent ductus arteriosus in preterm infants. Cochrane Database Syst Rev. 2008; (1):CD003951.9. Mosalli R, Alfaleh K, Paes B. Role of prophylactic surgical ligation of patent ductus arteriosus in extremely low birth weight infants: systematic review and implications for clinical practice. Ann Pediatr Cardiol. 2009; 2:120–126.10. Robie DK, Waltrip T, Garcia-Prats JA, Pokorny WJ, Jaksic T. Is surgical ligation of a patent ductus arteriosus the preferred initial approach for the neonate with extremely low birth weight? J Pediatr Surg. 1996; 31:1134–1137.11. Hsiao CC, Wung JT, Tsao LY, Chang WC. Early or late surgical ligation of medical refractory patent ductus arteriosus in premature infants. J Formos Med Assoc. 2009; 108:72–77.12. Jaillard S, Larrue B, Rakza T, Magnenant E, Warembourg H, Storme L. Consequences of delayed surgical closure of patent ductus arteriosus in very premature infants. Ann Thorac Surg. 2006; 81:231–234.13. Vida VL, Lago P, Salvatori S, Boccuzzo G, Padalino MA, Milanesi O, Speggiorin S, Stellin G. Is there an optimal timing for surgical ligation of patent ductus arteriosus in preterm infants? Ann Thorac Surg. 2009; 87:1509–1515.14. Waleh N, McCurnin DC, Yoder BA, Shaul PW, Clyman RI. Patent ductus arteriosus ligation alters pulmonary gene expression in preterm baboons. Pediatr Res. 2011; 69:212–216.15. Hamrick SE, Hansmann G. Patent ductus arteriosus of the preterm infant. Pediatrics. 2010; 125:1020–1030.16. Antonucci R, Bassareo P, Zaffanello M, Pusceddu M, Fanos V. Patent ductus arteriosus in the preterm infant: new insights into pathogenesis and clinical management. J Matern Fetal Neonatal Med. 2010; 23:34–37.17. Sehgal A, Ramsden CA, McNamara PJ. Indomethacin impairs coronary perfusion in infants with hemodynamically significant ductus arteriosus. Neonatology. 2012; 101:20–27.18. Benitz WE. Treatment of persistent patent ductus arteriosus in preterm infants: time to accept the null hypothesis? J Perinatol. 2010; 30:241–252.19. Benitz WE. Learning to live with patency of the ductus arteriosus in preterm infants. J Perinatol. 2011; 31:S42–S48.20. Bose CL, Laughon MM. Patent ductus arteriosus: lack of evidence for common treatments. Arch Dis Child Fetal Neonatal Ed. 2007; 92:F498–F502.21. Vanhaesebrouck S, Zonnenberg I, Vandervoort P, Bruneel E, Van Hoestenberghe MR, Theyskens C. Conservative treatment for patent ductus arteriosus in the preterm. Arch Dis Child Fetal Neonatal Ed. 2007; 92:F244–F247.22. McNamara PJ, Stewart L, Shivananda SP, Stephens D, Sehgal A. Patent ductus arteriosus ligation is associated with impaired left ventricular systolic performance in premature infants weighing less than 1000 g. J Thorac Cardiovasc Surg. 2010; 140:150–157.23. Noori S, Friedlich P, Seri I, Wong P. Changes in myocardial function and hemodynamics after ligation of the ductus arteriosus in preterm infants. J Pediatr. 2007; 150:597–602.24. Teixeira LS, Shivananda SP, Stephens D, Van Arsdell G, McNamara PJ. Postoperative cardiorespiratory instability following ligation of the preterm ductus arteriosus is related to early need for intervention. J Perinatol. 2008; 28:803–810.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk Factors of Failure of Ibuprofen Treatment in Preterm Infants with Hemodynamically Significant Patent Ductus Arteriosus
- Recent Advance in Management of Patent Ductus Arteriosus in Extremely Low Birth Weight Infants
- Aneurysm after Surgical Ligation of Patent Ductus Arteriosus: A Case Report
- Risk Factors and Neonatal Outcomes of Patent Ductus Arteriosus Ligation in Preterm Infants in a Single Center over 6 Years
- Three Cases of Hemolysis After Transcatheter Closure of A Patent Ductus Arteriosus