J Korean Soc Spine Surg.
2008 Sep;15(3):165-173. 10.4184/jkss.2008.15.3.165.
Usefulness of Coronal MR Image in Diagnosis of Foraminal and Extraforaminal Disc Herniation
- Affiliations
-
- 1Department of Orthopedic Surgery, Dankook University School of Medicine, Cheonan, Korea. osmin71@naver.com
- 2Department of Radiology, Dankook University School of Medicine, Cheonan, Korea.
- KMID: 1747200
- DOI: http://doi.org/10.4184/jkss.2008.15.3.165
Abstract
-
STUDY DESIGN: This is a retrospective study
OBJECTIVES
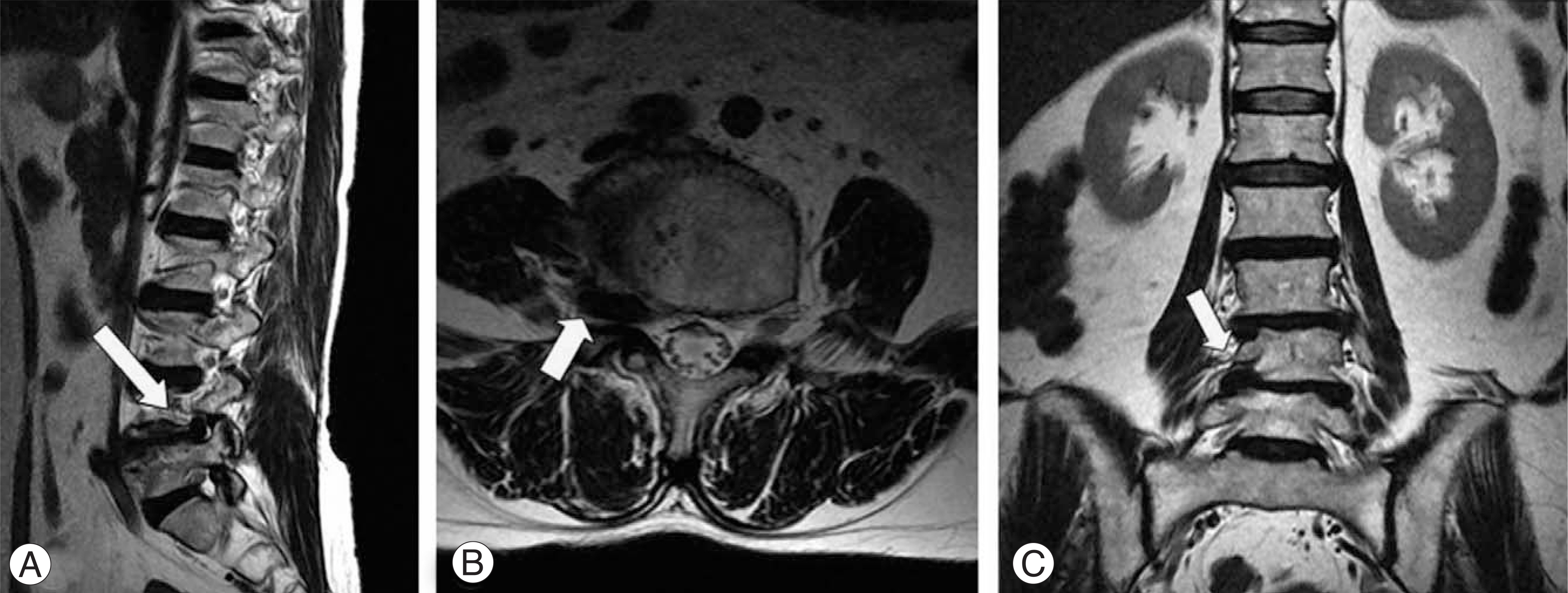
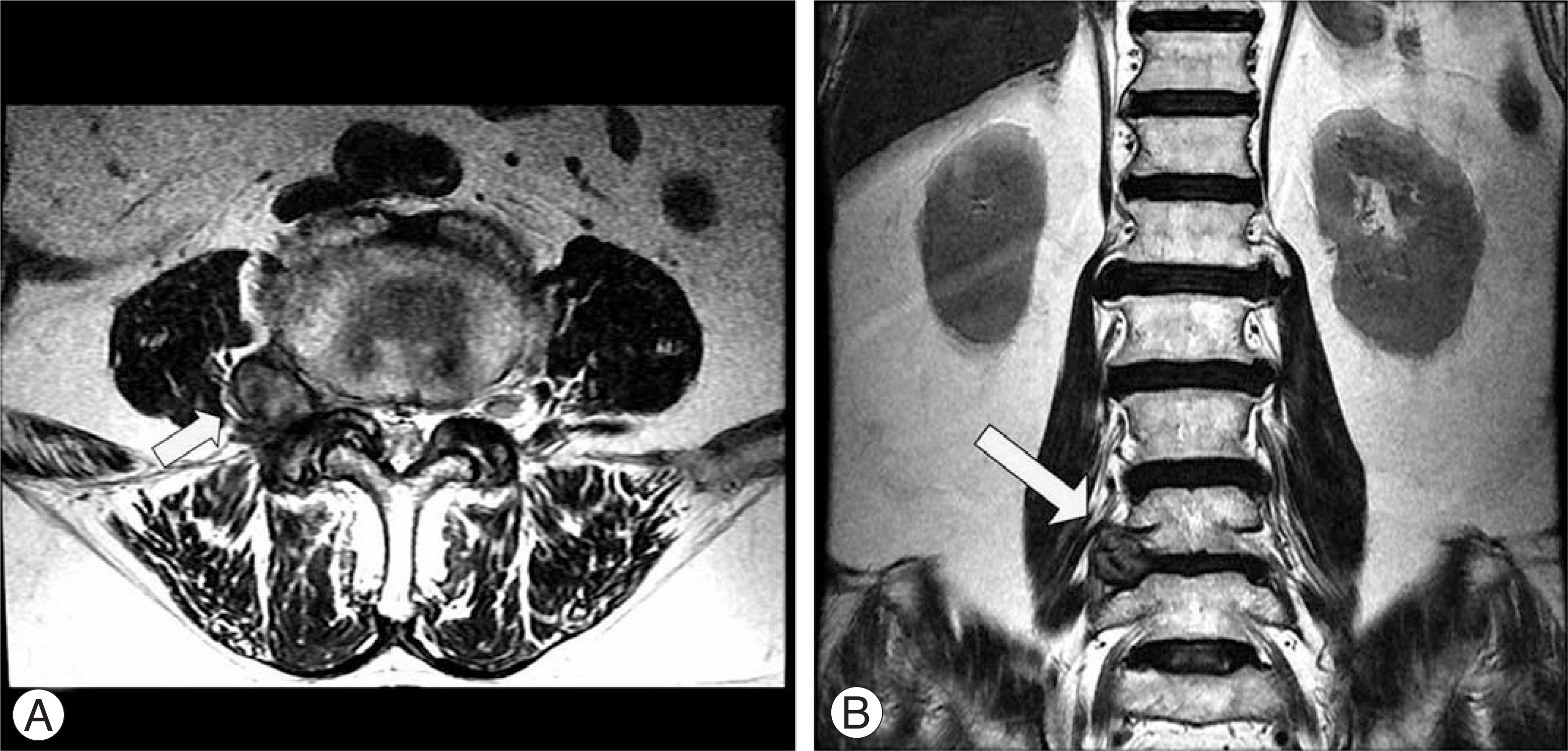
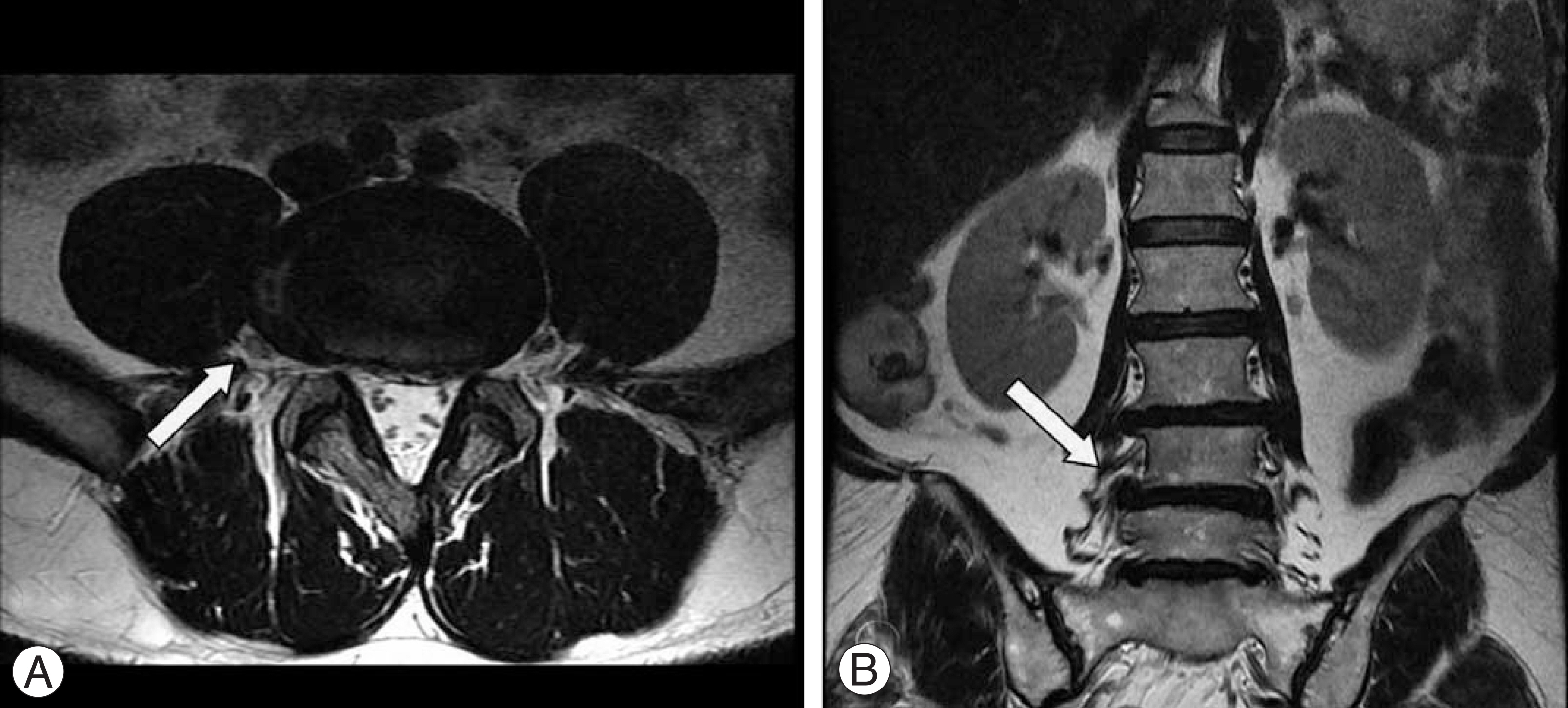
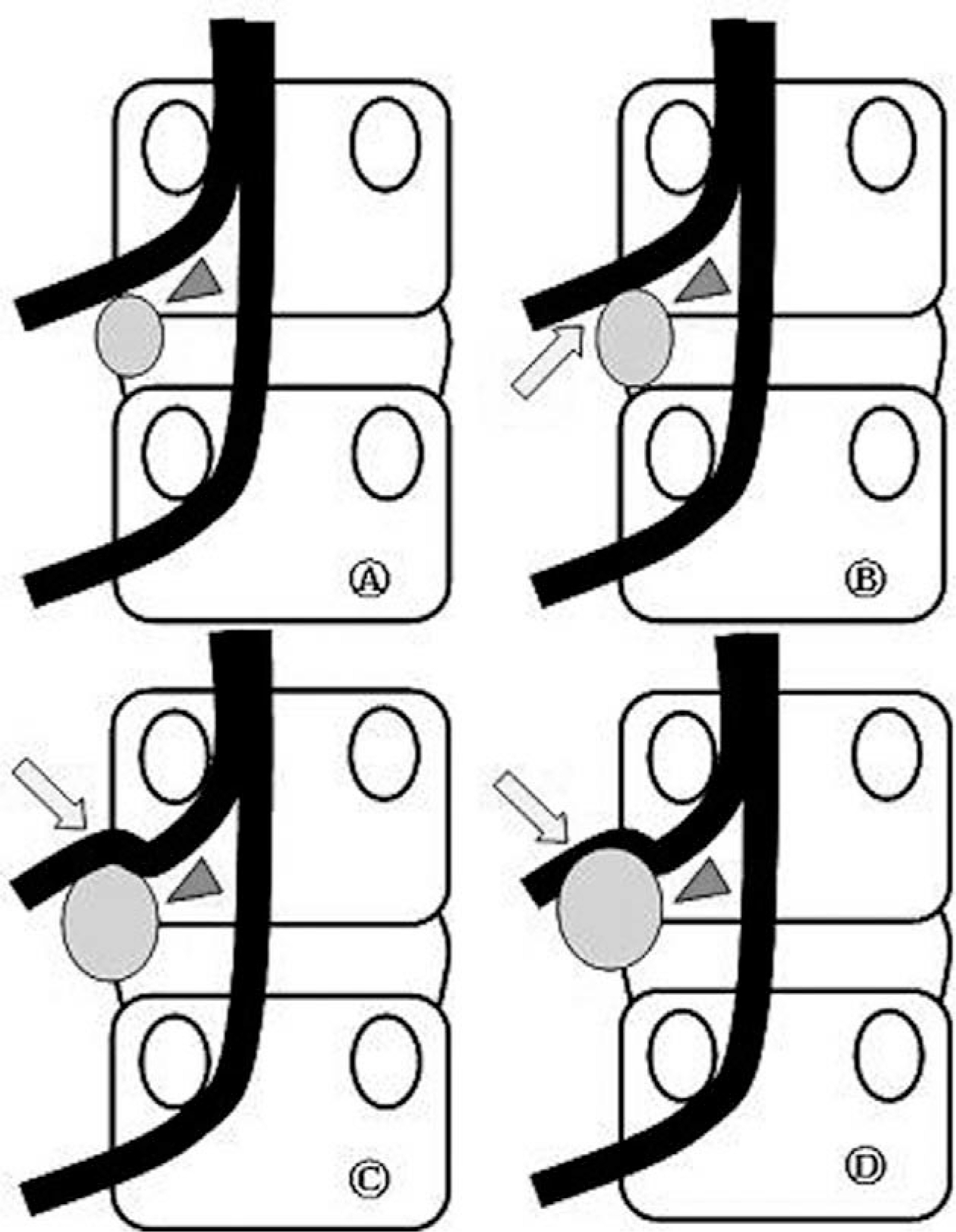
The coronal MR images were carefully evaluated to document the efficacy of diagnosing foraminal and extraforaminal disc herniations. SUMMARY OF LITERATURE REVIEW: Extraforaminal disc herniations constitute 1~11.7% of all disc herniations. The diagnosis of it demands great caution because it must be distinguished from intraspinal canal disc herniation. Diagnosing extraforaminal disc herniations can be neglected with using ordinary diagnostic methods.
MATERIALS AND METHODS
A retrospective analysis was performed on 24 patients, (26 cases) that underwent lumbar spine MRI, with the T2 coronal images, for the evaluation of disc herniations from March 2006 to March 2007. Every MRI image of each patient who had foraminal or extraforaminal disc herniations was graded according to the Pfirrmann's classification of diagnostic efficacy by two spinal surgery specialists and two radiology specialists.
RESULTS
There were 13 cases of foraminal disc herniation and 13 cases of extraforaminal disc herniation in all 26 cases that were diagnosed by MRI. The coronal and axial images were more effective than the sagittal images for the discrimination of a compressed root. Especially, for the extraforaminal disc herniation, all of the coronal images were graded as grade 3; on the other hand, all of the sagittal images were not helpful for the assessment and the axial images were graded as grade 2 for 38.5% of the and as grade 3 for 61.5%. So, the coronal images were most effective for making the diagnosis of extraforaminal disc herniation and this was statistically significant (p<0.05).
CONCLUSION
For the accurate discrimination of the location and the grading of foraminal and extraforaminal disc herniation, MRI, and especially the coronal images, is an effective and useful method in addition to conducting a physical examination.
Figure
Cited by 2 articles
-
Relative Risk of Operation between Lumbar Far Lateral Disc Herniation and Posterolateral Disc Herniation: A Retrospective Cohort Study
Dae Ho Ha, Dae Moo Shim, Tae Kyun Kim, Sung Kyun Oh, Jin Kim
J Korean Orthop Assoc. 2017;52(5):442-447. doi: 10.4055/jkoa.2017.52.5.442.Usefulness of the ProSet MRI for Diagnosis of the Extraforaminal Disc Herniation
Myun-Whan Ahn, Ui-Sik Kim, Gi-Beom Kim
J Korean Soc Spine Surg. 2013;20(1):28-33. doi: 10.4184/JKSS.2021.20.1.28.
Reference
-
1). Epstein NE, Epstein JA, Carras R, Hyman RA. Fal lateral disc herniations and associated structural abnormial-ities. An evaluation in 60 patients of the comparative value of CT, MRI, and myelo-CT in diagnosis and management, Spine. 1990; 15:534–539.2). Jackson RP, Glah JJ. Foraminal and extraforaminal lumbar disc herniation: Diagnosis and treatment. Spine. 1982; 12:577–585.
Article3). Junichi K, Mitsuo H. Diagnosis and operative treatment of intraforaminal and extraforaminal nerve root compression. Spine. 1991; 16:1312–1320.
Article4). MacNab I. Negative disc exploration. An analysis of the causes of sixty-eight patients. J Bone Joint Surg Am. 1971; 53:891–903.5). Abdullah AF, Ditto EW, Byrd EB, Williams R. Extreme-lateral lumbar disc herniations. Clinical syndrome and special problems of disagnosis. J. Neurosurg. 1974; 41:229–234.6). Chang H, Park JB, Lee IJ, et al. Diagnosis and treatment for the extraforaminal lumbar disc herniation, J Korea Soc Spine Surg. 1998; 1:102–108.7). Kornberg M. Extreme lateral lumbar disc herniations. Clinical syndrome and computed tomography recognition. Spine. 1987; 12:586–589.8). Zindrick MR, Wiltse LL, Rauschning W. Disc herniations lateral to the intervertebral foramen. Lumbar Spine Surgery. St. Louis: C.V. Mosby Co;p. 195. 1987.9). Godersky JC, Erickson DL, Seljeskog EL. Extreme lateral disc herniation: Diagnosis by computed tomographic scanning. Neurosurg. 1984; 14:549–552.
Article10). Kornberg M. Extreme lateral lumbar disc herniations. Clinical syndrome and computed tomography recognition. Spine. 1987; 12:586–589.11). Pfirrmann CW, Dora C, Schmid MR, Zanetto M, Hodler J, Boos N. MR image-based grading of lumbar nerve root compression due to disk herniation: reliability study with surgical correlation. Radiology. 2004; 230:583–588.12). Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979; 86:420–428.
Article13). Bronx NY. Foraminal and far lateral lumbar disc herniations: Surgical alternatives outcome measures. Spinal Cord. 2002; 40:491–500.14). Greiner-Perth R, Bohm H, Allam Y. A new technique for the treatment of lumbar far lateral disc herniation: technical note and preliminary results. Eur Spine J. 2003; 12:320–324.
Article15). Faust SE, Ducker TB, VanHassent JA. Lateral lumbar disc herniations. J Spinal Disord. 1992; 5:97–103.
Article16). Epstein NE. Different surgical approaches to far lateral lumbar disc herniations. J Spinal Disord. 1995; 8:383–394.
Article17). Bogduk N, Twomey L. Clinical Anatomy of the Spine. Edinburgh: Churchill Livingstone;1987.18). Bose K, Balasubramaniam P. Nerve root canals of the lumbar spine. Spine. 1984; 9:16–18.
Article19). Abdullah AF, Wolber PGH, Warfield JR, Gunadi IK. Surgical management of extreme lateral lumbar disc herniations: review of 138 cases. Neurosurgery. 1988; 22:648–653.
Article20). Lee CK, Rauschning W, Glenn W. Lateral lumbar canal stenosis: Classification, pathologic anatomy and surgical decompression. Spine. 1988; 13:313–320.21). Spencer DL, Irwin GS, Miller JAA. Anatomy and significance of fixation of the lumbosacral nerve roots in sciatica. Spine. 1983; 6:672–695.
Article22). Sheehan JM, Shaffrey CI, Jane JA. Degenerative lumbar stenosis. Clnical orthopaedics and related research. 2001; 384:61–74.
Article23). O'Brien MF, Peterson D, Crockard HA. A prosterolateral microsurgical approach to extremelateral lumbar disc herniation. J Neurosurg. 1995; 83:636–640.24). Forristal RM, Marsh HO, Pay NT. MRI & CT of the lumbar spine. Comparison of diagnotic methods and correlation with surgical findings. Spine. 1988; 13:1049–1054.25). Modic MT, Masarynk T, Boumphrey F, et al. Lumbar herniated disc disease and canal stenosis. AJNR. 1986; 7:709–717.26). Mikael MA. High resolution computed tomography in the diagnosis of laterally herniated lumbar disc. Comput Radiol. 1983; 7:161–166.27). Maroon JC, Kopitnik TA, Schulhof LA, Abla A. Diagnosis and microsurgical approach to far-lateral disc herniation in the lumbar spine. J Neurosurg. 1990; 72:378–382.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usefulness of the ProSet MRI for Diagnosis of the Extraforaminal Disc Herniation
- Morphologic Changes of L5 Root at Coronal Source Images of MR Myelography in Cases of Foraminal or Extraforaminal Compression
- Diagnosis of Lumbar Lateral Disc Herniation: Value of Magnetic Resonance Imaging Revisited
- Paramedian Tangential Approach for the Lumbosacral Extraforaminal Disc Herniations
- Lateral Lumbar Disc Herniation: MR Imaging Findings and Correlation with Clinical Symptoms