Clin Orthop Surg.
2011 Sep;3(3):217-224. 10.4055/cios.2011.3.3.217.
Technique and Early Results of Percutaneous Reduction of Sagittally Unstable Intertrochateric Fractures
- Affiliations
-
- 1Department of Orthopedic Surgery, Kyung Hee University Hospital at Gangdong, Seoul, Korea. khrhyu@gmail.com
- 2Department of Orthopedic Surgery, Kyung Hee University Hospital, Seoul, Korea.
- KMID: 1743912
- DOI: http://doi.org/10.4055/cios.2011.3.3.217
Abstract
- BACKGROUND
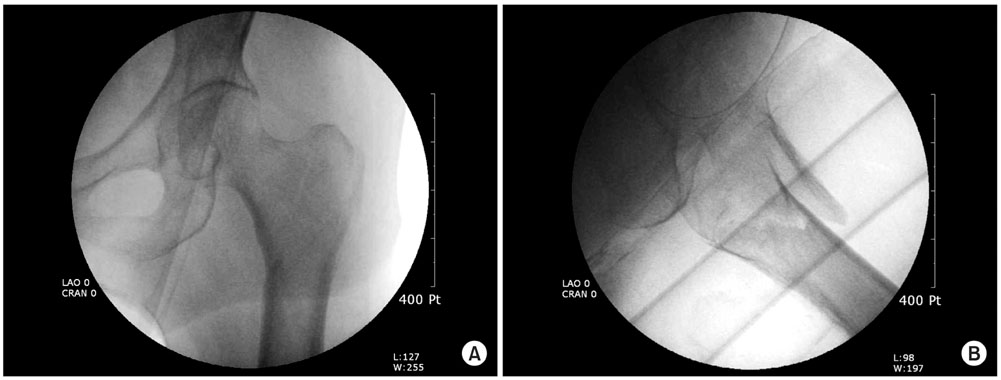
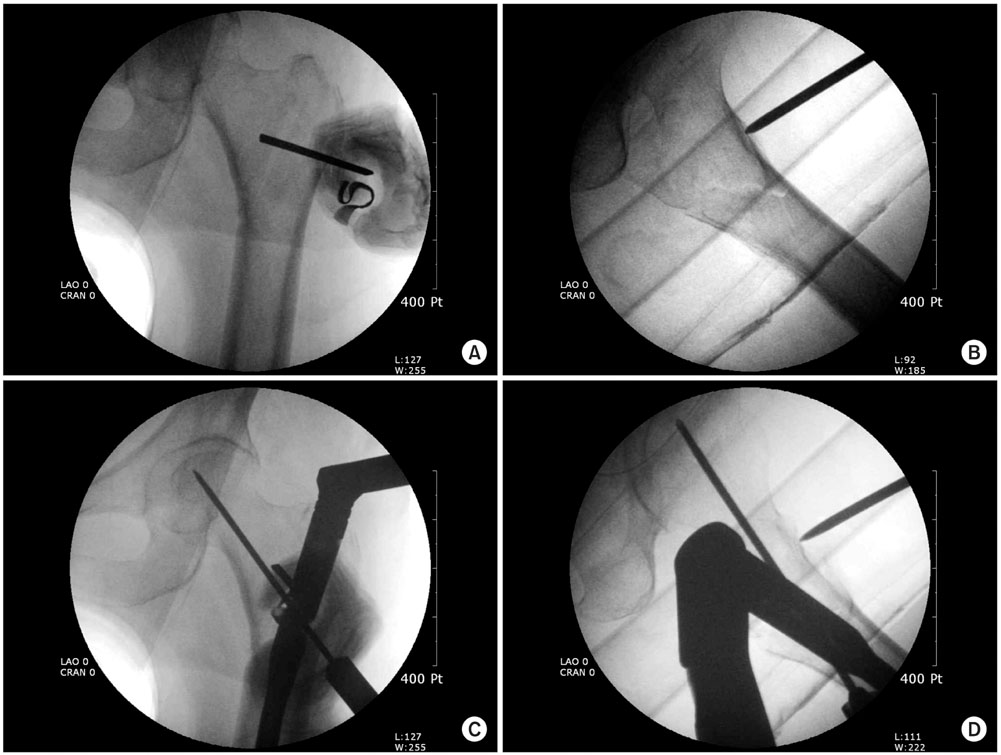
This paper introduces a percutaneous reduction technique using one or two Steinman pin(s) to reduce sagittally unstable intertrochanteric fractures.
METHODS
A fracture was defined as a sagittally unstable intertrochanteric fracture when posterior sagging of a distal fragment and flexion of the proximal fragment worsens after usual maneuvers for a closed reduction. Of 119 intertrochanteric fractures treated from June 2007 to December 2008, twenty-one hips showed sagittal instability. The sagittal displacement was reduced using a Steinmann pin as a joystick, and stabilized with a nail device. Nineteen hips were followed up for more than one year. The clinical and radiological results were reviewed in 19 hips and compared with those of the remaining cases.
RESULTS
The demographics were similar in both groups. The mean anesthetic time did not differ. Although the pre-injury and final activity levels were significantly lower in the study group, the degree of recovery was the same. No clinical complications related to this technique were encountered. Radiologically, the reduction was good in all hips in both groups. Union was obtained in all cases without any time differences.
CONCLUSIONS
This less invasive reduction technique is simple and safe to use for this type of difficult fracture.
MeSH Terms
Figure
Cited by 1 articles
-
Risk Factors Associated with Failure of Cephalomedullary Nail Fixation in the Treatment of Trochanteric Hip Fractures
Jehyun Yoo, Jundong Chang, Changwon Park, Jihyo Hwang
Clin Orthop Surg. 2020;12(1):29-36. doi: 10.4055/cios.2020.12.1.29.
Reference
-
1. Hornby R, Evans JG, Vardon V. Operative or conservative treatment for trochanteric fractures of the femur: a randomised epidemiological trial in elderly patients. J Bone Joint Surg Br. 1989. 71(4):619–623.
Article2. Lorich DG, Geller DS, Nielson JH. Osteoporotic pertrochanteric hip fractures: management and current controversies. Instr Course Lect. 2004. 53:441–454.3. Chang WS, Zuckerman JD, Kummer FJ, Frankel VH. Biomechanical evaluation of anatomic reduction versus medial displacement osteotomy in unstable intertrochanteric fractures. Clin Orthop Relat Res. 1987. (225):141–146.
Article4. Desjardins AL, Roy A, Paiement G, et al. Unstable intertrochanteric fracture of the femur: a prospective randomised study comparing anatomical reduction and medial displacement osteotomy. J Bone Joint Surg Br. 1993. 75(3):445–447.
Article5. Carr JB. The anterior and medial reduction of intertrochanteric fractures: a simple method to obtain a stable reduction. J Orthop Trauma. 2007. 21(7):485–489.
Article6. Nam WD, Kim IY, Rhyu KH. Blood loss and transfusion in primary total hip arthroplasty. J Korean Hip Soc. 2006. 18(1):1–5.
Article7. Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD. Ambulatory ability after hip fracture: a prospective study in geriatric patients. Clin Orthop Relat Res. 1995. (310):150–159.8. Kim SI, Park MH, Han KS. Transfusion medicine. 1999. 2nd ed. Seoul: Medical Book Publisher Co..9. Fogagnolo F, Kfuri M Jr, Paccola CA. Intramedullary fixation of pertrochanteric hip fractures with the short AO-ASIF proximal femoral nail. Arch Orthop Trauma Surg. 2004. 124(1):31–37.
Article10. Evans EM. The treatment of trochanteric fractures of the femur. J Bone Joint Surg Br. 1949. 31(2):190–203.
Article11. Boyd HB, Griffin LL. Classification and treatment of trochanteric fractures. Arch Surg. 1949. 58(6):853–866.
Article12. Fracture and dislocation compendium. Orthopaedic Trauma Association Committee for Coding and Classification. J Orthop Trauma. 1996. 10:Suppl 1. v–ix. 1–154.13. Said GZ, Farouk O, Said HG. An irreducible variant of intertrochanteric fractures: a technique for open reduction. Injury. 2005. 36(7):871–874.
Article14. Moehring HD, Nowinski GP, Chapman MW, Voigtlander JP. Irreducible intertrochanteric fractures of the femur. Clin Orthop Relat Res. 1997. (339):197–199.
Article15. Koval KJ, Zuckerman JD. Bucholz RW, Heckman JD, editors. Intertrochanteric fractures. Fractures in adults. 2001. 5th ed. Philadelphia: Lippincott Williams & Wilkins;1635–1663.
Article16. Anglen JO, Baumgaertner MR, Smith WR, Tornetta Iii P, Ziran BH. Technical tips in fracture care: fractures of the hip. Instr Course Lect. 2008. 57:17–24.17. Byrd JW. Hip arthroscopy utilizing the supine position. Arthroscopy. 1994. 10(3):275–280.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of unstable open and closed Tibial Fractures using the Ilizarov Method
- Closed Reduction and Percutaneous Fixation in the Treatment of Proximal Humerus Fractures
- Percutaneous Pinning & External Fixation In the Treatment of Proximal Humerus Fracture
- Surgical Treament for Unstable Intra-articular Fracture of the Distal Radius with Rayhack's Transulnar Percutaneous Pinning Technique
- Management of Unstable Proximal Tibial Fractures Using the Ilizarov