Clin Orthop Surg.
2014 Mar;6(1):62-71. 10.4055/cios.2014.6.1.62.
Determining the Best Treatment for Simple Bone Cyst: A Decision Analysis
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. pmsmed@gmail.com
- 2Department of Orthopaedic Surgery, Myongji Hospital, Kwandong University College of Medicine, Goyang, Korea.
- 3Department of Orthopedic Surgery, Seoul National University Children's Hospital, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 1737633
- DOI: http://doi.org/10.4055/cios.2014.6.1.62
Abstract
- BACKGROUND
The treatment of simple bone cysts (SBC) in children varies significantly among physicians. This study examined which procedure is better for the treatment of SBC, using a decision analysis based on current published evidence.
METHODS
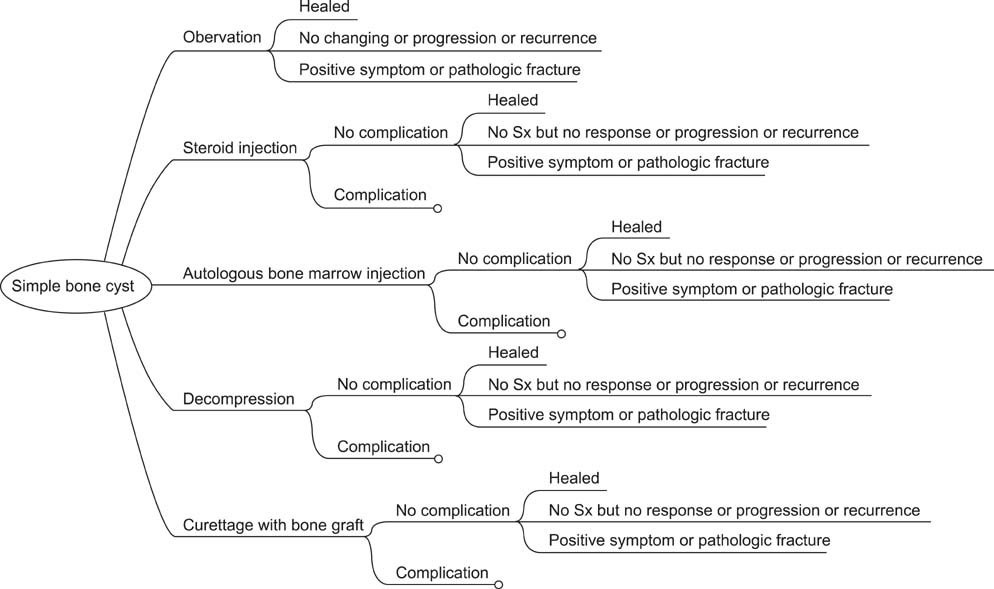
A decision tree focused on five treatment modalities of SBC (observation, steroid injection, autologous bone marrow injection, decompression, and curettage with bone graft) were created. Each treatment modality was further branched, according to the presence and severity of complications. The probabilities of all cases were obtained by literature review. A roll back tool was utilized to determine the most preferred treatment modality. One-way sensitivity analysis was performed to determine the threshold value of the treatment modalities. Two-way sensitivity analysis was utilized to examine the joint impact of changes in probabilities of two parameters.
RESULTS
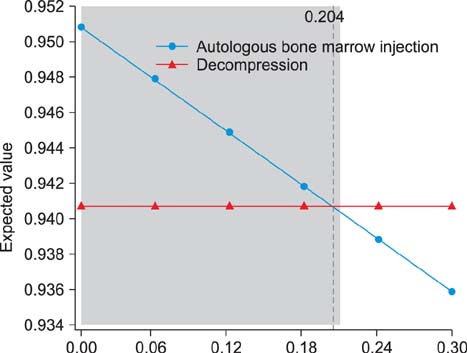
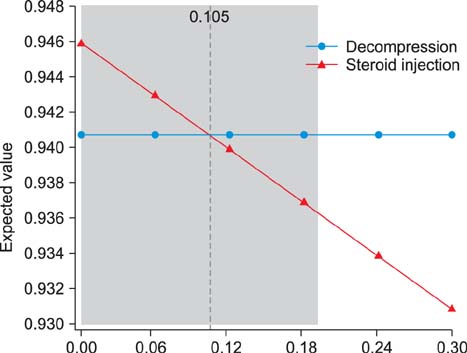
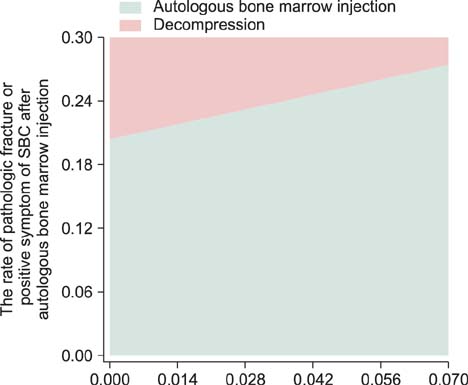
The decision model favored autologous bone marrow injection. The expected value of autologous bone marrow injection was 0.9445, while those of observation, steroid injection, decompression, and curettage and bone graft were 0.9318, 0.9400, 0.9395, and 0.9342, respectively. One-way sensitivity analysis showed that autologous bone marrow injection was better than that of decompression for the expected value when the rate of pathologic fracture, or positive symptoms of SBC after autologous bone marrow injection, was lower than 20.4%.
CONCLUSIONS
In our study, autologous bone marrow injection was found to be the best choice of treatment of SBC. However, the results were sensitive to the rate of pathologic fracture after treatment of SBC. Physicians should consider the possibility of pathologic fracture when they determine a treatment method for SBC.
MeSH Terms
Figure
Cited by 1 articles
-
Therapeutic Approach to Humeral Pathologic Fracture Caused by Benign Bone Tumor
Jeung Il Kim, Um Ji Kim, Nam Hoon Moon, Hui Taek Kim, Tae Young Ahn, In Sook Lee, You Seon Song, Kyung Un Choi
J Korean Orthop Assoc. 2016;51(6):509-514. doi: 10.4055/jkoa.2016.51.6.509.
Reference
-
1. Wilkins RM. Unicameral bone cysts. J Am Acad Orthop Surg. 2000; 8(4):217–224.2. Bernstein J. Decision analysis. J Bone Joint Surg Am. 1997; 79(9):1404–1414.3. Park MS, Chung CY, Kwon DG, Sung KH, Choi IH, Lee KM. Prophylactic femoral varization osteotomy for contralateral stable hips in non-ambulant individuals with cerebral palsy undergoing hip surgery: decision analysis. Dev Med Child Neurol. 2012; 54(3):231–239.4. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007; 147(8):573–577.5. Kaelin AJ, MacEwen GD. Unicameral bone cysts: natural history and the risk of fracture. Int Orthop. 1989; 13(4):275–282.6. Farber JM, Stanton RP. Treatment options in unicameral bone cysts. Orthopedics. 1990; 13(1):25–32.7. Lokiec F, Ezra E, Khermosh O, Wientroub S. Simple bone cysts treated by percutaneous autologous marrow grafting: a preliminary report. J Bone Joint Surg Br. 1996; 78(6):934–937.8. Docquier PL, Delloye C. Treatment of simple bone cysts with aspiration and a single bone marrow injection. J Pediatr Orthop. 2003; 23(6):766–773.9. Abdel-Wanis ME, Tsuchiya H, Uehara K, Tomita K. Minimal curettage, multiple drilling, and continuous decompression through a cannulated screw for treatment of calcaneal simple bone cysts in children. J Pediatr Orthop. 2002; 22(4):540–543.10. Roposch A, Saraph V, Linhart WE. Treatment of femoral neck and trochanteric simple bone cysts. Arch Orthop Trauma Surg. 2004; 124(7):437–442.11. Kokavec M, Fristakova M, Polan P, Bialik GM. Surgical options for the treatment of simple bone cyst in children and adolescents. Isr Med Assoc J. 2010; 12(2):87–90.12. Canavese F, Wright JG, Cole WG, Hopyan S. Unicameral bone cysts: comparison of percutaneous curettage, steroid, and autologous bone marrow injections. J Pediatr Orthop. 2011; 31(1):50–55.13. Cha SM, Shin HD, Kim KC, Hwang JM, Kim BK. Outcomes from treatment of simple bone cyst in the long bones with flexible intramedullary nailing in children and adolescents: a retrospective cases series. J Korean Orthop Assoc. 2012; 47(3):178–184.14. Baek SG, Oh CW, Jeon IH, Min WK, Park IH. Comparison of results by its location and treatment modality of the simple bone cyst. J Korean Musculoskelet Transplant Soc. 2006; 6(2):88–97.15. Gonzalez LP, Pignaton W, Kusano PS, Modolo NS, Braz JR, Braz LG. Anesthesia-related mortality in pediatric patients: a systematic review. Clinics (Sao Paulo). 2012; 67(4):381–387.16. Stadler M, Bardiau F, Seidel L, Albert A, Boogaerts JG. Difference in risk factors for postoperative nausea and vomiting. Anesthesiology. 2003; 98(1):46–52.17. Hines R, Barash PG, Watrous G, O'Connor T. Complications occurring in the postanesthesia care unit: a survey. Anesth Analg. 1992; 74(4):503–509.18. Apfel CC, Kranke P, Eberhart LH. Comparison of surgical site and patient's history with a simplified risk score for the prediction of postoperative nausea and vomiting. Anaesthesia. 2004; 59(11):1078–1082.19. van Kasteren ME, Mannien J, Ott A, Kullberg BJ, de Boer AS, Gyssens IC. Antibiotic prophylaxis and the risk of surgical site infections following total hip arthroplasty: timely administration is the most important factor. Clin Infect Dis. 2007; 44(7):921–927.20. Abu Hanifah Y. Post-operative surgical wound infection. Med J Malaysia. 1990; 45(4):293–297.21. Dhillon KS, Kok CS. The incidence of post-operative wound infection in orthopaedic surgery. Med J Malaysia. 1995; 50(3):237–240.22. Pittet D, Harbarth S, Ruef C, et al. Prevalence and risk factors for nosocomial infections in four university hospitals in Switzerland. Infect Control Hosp Epidemiol. 1999; 20(1):37–42.23. National Nosocomial Infections Surveillance (NNIS) System report, data summary from October 1986-April 1998, issued June 1998. Am J Infect Control. 1998; 26(5):522–533.24. Shrier I, Matheson GO, Kohl HW 3rd. Achilles tendonitis: are corticosteroid injections useful or harmful? Clin J Sport Med. 1996; 6(4):245–250.25. Hagmann S, Eichhorn F, Moradi B, et al. Mid- and long-term clinical results of surgical therapy in unicameral bone cysts. BMC Musculoskelet Disord. 2011; 12:281.26. Sung AD, Anderson ME, Zurakowski D, Hornicek FJ, Gebhardt MC. Unicameral bone cyst: a retrospective study of three surgical treatments. Clin Orthop Relat Res. 2008; 466(10):2519–2526.27. Yandow SM, Marley LD, Fillman RR, Galloway KS. Precordial Doppler evaluation of simple bone cyst injection. J Pediatr Orthop. 2009; 29(2):196–200.28. Abril JC, Queiruga JA, Casas J, Albinana J. Unusual finding after contrast injection of a solitary bone cyst: a case report. Acta Orthop Belg. 1999; 65(2):235–238.29. Kim DH, Rhim R, Li L, et al. Prospective study of iliac crest bone graft harvest site pain and morbidity. Spine J. 2009; 9(11):886–892.