Korean J Lab Med.
2011 Jul;31(3):205-211. 10.3343/kjlm.2011.31.3.205.
Streptococcus suis Meningitis with Bilateral Sensorineural Hearing Loss
- Affiliations
-
- 1Department of Laboratory Medicine and Genetics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. micro.lee@samsung.com
- 2Department of Infectious Diseases, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1735856
- DOI: http://doi.org/10.3343/kjlm.2011.31.3.205
Abstract
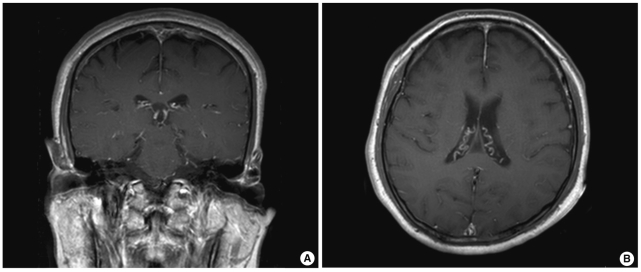
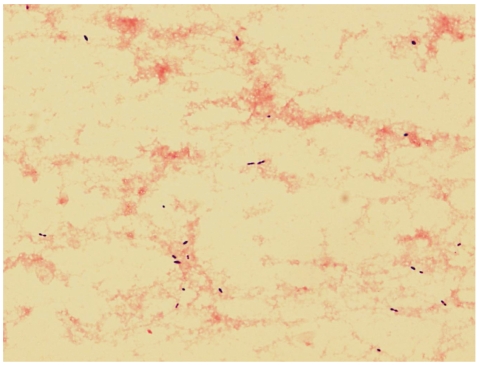
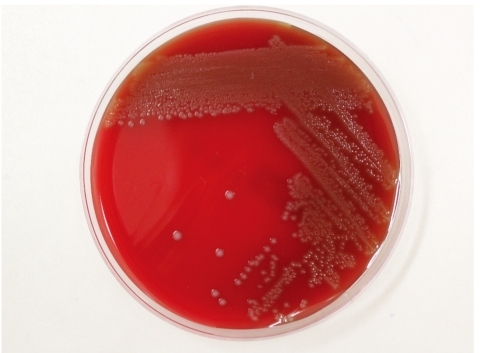
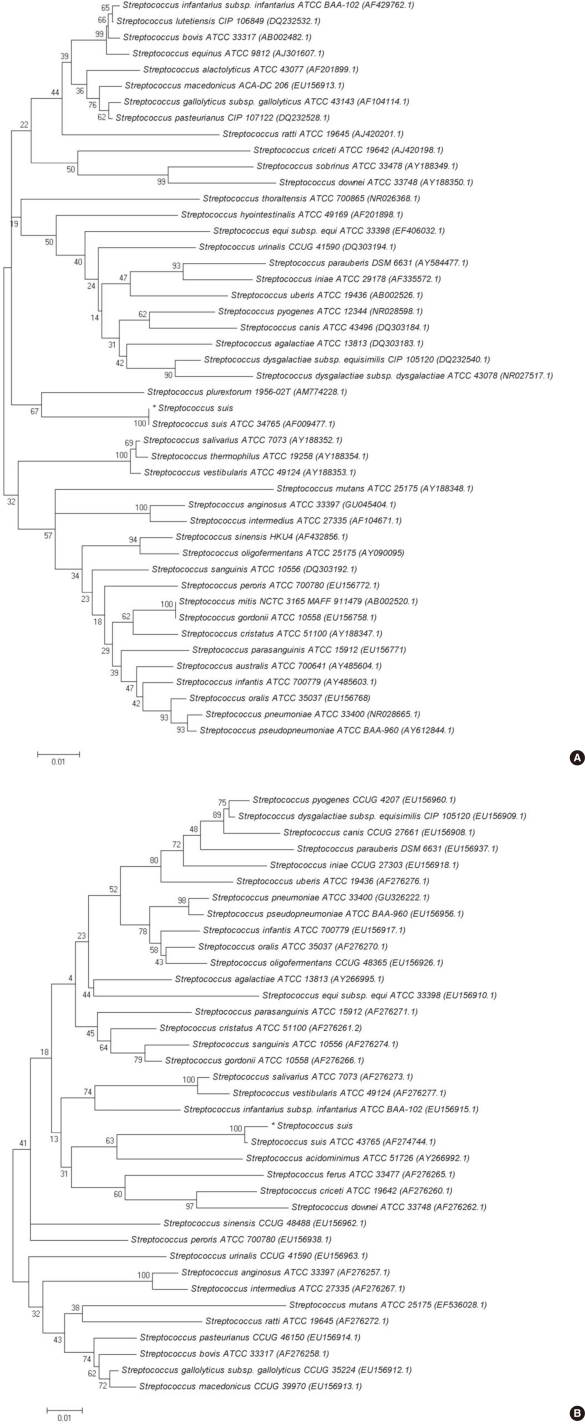
- Streptococcus suis infection is an emerging zoonosis in Asia. The most common disease manifestation is meningitis, which is often associated with hearing loss and cochleovestibular signs. S. suis infection in humans mainly occurs among risk groups that have frequent exposure to pigs or raw pork. Here, we report a case of S. suis meningitis in a 67-yr-old pig carcass handler, who presented with dizziness and sensorineural hearing loss followed by headaches. Gram-positive diplococci were isolated from cerebrospinal fluid (CSF) and blood cultures and showed gray-white colonies with alpha-hemolysis. S. suis was identified from CSF and blood cultures by using a Vitek 2 system (bioMerieux, France), API 20 STREP (bioMerieux), and performing 16S rRNA and tuf gene sequencing. Even after receiving antibiotic treatment, patients with S. suis infection frequently show complications such as hearing impairment and vestibular dysfunction. To the best of our knowledge, this is the first case of S. suis meningitis in Korea. Prevention through public health surveillance is recommended, especially for individuals who have occupational exposures to swine and raw pork.
Keyword
MeSH Terms
-
Aged
Animals
Bacterial Proteins/genetics
Blood/microbiology
Cerebrospinal Fluid/microbiology
Hearing Loss, Bilateral/complications/*diagnosis/microbiology
Humans
Male
Meningitis, Bacterial/complications/*diagnosis/microbiology
Phylogeny
RNA, Ribosomal, 16S/genetics
Sequence Analysis, DNA
Streptococcus suis/classification/genetics/*isolation & purification
Swine
Tomography, X-Ray Computed
Figure
Reference
-
1. Lun ZR, Wang QP, Chen XG, Li AX, Zhu XQ. Streptococcus suis: an emerging zoonotic pathogen. Lancet Infect Dis. 2007; 7:201–209. PMID: 17317601.2. Wertheim HF, Nghia HD, Taylor W, Schultsz C. Streptococcus suis: an emerging human pathogen. Clin Infect Dis. 2009; 48:617–625. PMID: 19191650.3. Tan JH, Yeh BI, Seet CS. Deafness due to haemorrhagic labyrinthi tis and a review of relapses in Streptococcus suis meningitis. Singapore Med J. 2010; 51:e30–e33. PMID: 20358139.4. Wangkaew S, Chaiwarith R, Tharavichitkul P, Supparatpinyo K. Streptococcus suis infection: a series of 41 cases from Chiang Mai University Hospital. J Infect. 2006; 52:455–460. PMID: 16690131.5. Perch B, Kristjansen P, Skadhauge K. Group R streptococci pathogenic for man. Two cases of meningitis and one fatal case of sepsis. Acta Pathol Microbiol Scand. 1968; 74:69–76. PMID: 5700279.6. Clinical and Laboratory Standards Institute. Interpretive criteria for identification of bacteria and fungi by DNA target sequencing; approved guideline. Document MM18-A. 2008. Wayne, PA: Clinical and Laboratory Standards Institute.7. Aiyar A. The use of CLUSTAL W and CLUSTAL X for multiple sequence alignment. Methods Mol Biol. 2000; 132:221–241. PMID: 10547838.
Article8. Saitou N, Nei M. The neighbor-joining method: a new method for reconstructing phylogenetic trees. Mol Biol Evol. 1987; 4:406–425. PMID: 3447015.9. Kimura M. A simple method for estimating evolutionary rates of base substitutions through comparative studies of nucleotide sequences. J Mol Evol. 1980; 16:111–120. PMID: 7463489.
Article10. Tamura K, Dudley J, Nei M, Kumar S. MEGA4: Molecular Evolutionary Genetics Analysis (MEGA) software version 4.0. Mol Biol Evol. 2007; 24:1596–1599. PMID: 17488738.
Article11. Gottschalk M, Segura M. The pathogenesis of the meningitis caused by Streptococcus suis: the unresolved questions. Vet Microbiol. 2000; 76:259–272. PMID: 10973700.12. Facklam R. What happened to the streptococci: overview of taxonomic and nomenclature changes. Clin Microbiol Rev. 2002; 15:613–630. PMID: 12364372.
Article13. Heidt MC, Mohamed W, Hain T, Vogt PR, Chakraborty T, Do-mann E. Human infective endocarditis caused by Streptococcus suis serotype 2. J Clin Microbiol. 2005; 43:4898–4901. PMID: 16145171.14. Donsakul K, Dejthevaporn C, Witoonpanich R. Streptococcus suis infection: clinical features and diagnostic pitfalls. Southeast Asian J Trop Med Public Health. 2003; 34:154–158. PMID: 12971528.15. Wisselink HJ, Joosten JJ, Smith HE. Multiplex PCR assays for simultaneous detection of six major serotypes and two virulence-associated phenotypes of Streptococcus suis in tonsillar specimens from pigs. J Clin Microbiol. 2002; 40:2922–2929. PMID: 12149353.16. Smith HE, Veenbergen V, van der Velde J, Damman M, Wisselink HJ, Smits MA. The cps genes of Streptococcus suis serotypes 1, 2, and 9: development of rapid serotype-specific PCR assays. J Clin Microbiol. 1999; 37:3146–3152. PMID: 10488168.17. Lee GT, Chiu CY, Haller BL, Denn PM, Hall CS, Gerberding JL. Streptococcus suis meningitis, United States. Emerg Infect Dis. 2008; 14:183–185. PMID: 18258107.18. Kopić J, Paradzik MT, Pandak N. Streptococcus suis infection as a cause of severe illness: 2 cases from Croatia. Scand J Infect Dis. 2002; 34:683–684. PMID: 12374361.19. Willenburg KS, Sentochnik DE, Zadoks RN. Human Streptococcus suis meningitis in the United States. N Engl J Med. 2006; 354:1325. PMID: 16554543.20. Kim H, Lee SH, Moon HW, Kim JY, Hur M, Yun YM. Streptococcus suis Causes Septic Arthritis and Bacteremia: Phenotypic Characterization and Molecular Confirmation. Korean J Lab Med. 2011; 31:115–117. PMID: 21474987.21. Yu H, Jing H, Chen Z, Zheng H, Zhu X, Wang H, et al. Human Streptococcus suis outbreak, Sichuan, China. Emerg Infect Dis. 2006; 12:914–920. PMID: 16707046.22. Kay R, Cheng AF, Tse CY. Streptococcus suis infection in Hong Kong. QJM. 1995; 88:39–47. PMID: 7894987.23. Mai NT, Hoa NT, Nga TV, Linh le D, Chau TT, Sinh DX, et al. Streptococcus suis meningitis in adults in Vietnam. Clin Infect Dis. 2008; 46:659–667. PMID: 19413493.24. Ma E, Chung PH, So T, Wong L, Choi KM, Cheung DT, et al. Streptococcus suis infection in Hong Kong: an emerging infectious disease? Epidemiol Infect. 2008; 136:1691–1697. PMID: 18252026.25. Huang YT, Teng LJ, Ho SW, Hsueh PR. Streptococcus suis infection. J Microbiol Immunol Infect. 2005; 38:306–313. PMID: 16211137.26. Strupp M, Arbusow V, Maag KP, Gall C, Brandt T. Vestibular exercises improve central vestibulospinal compensation after vestibular neuritis. Neurology. 1998; 51:838–844. PMID: 9748036.
Article27. Halaby T, Hoitsma E, Hupperts R, Spanjaard L, Luirink M, Jacobs J. Streptococcus suis meningitis, a poacher's risk. Eur J Clin Microbiol Infect Dis. 2000; 19:943–945. PMID: 11205632.28. Greenwood BM. Corticosteroids for acute bacterial meningitis. N Engl J Med. 2007; 357:2507–2509. PMID: 18077815.
Article29. Durand F, Perino CL, Recule C, Brion JP, Kobish M, Guerber F, et al. Bacteriological diagnosis of Streptococcus suis meningitis. Eur J Clin Microbiol Infect Dis. 2001; 20:519–521. PMID: 11561816.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Cryptococcal Meningitis Presenting as Bilateral Sensorineural Hearing Loss
- Meningitis Caused by Streptococcus suis: Case Report and Review of the Literature
- Streptococcus suis causes bacterial meningitis with hearing loss in patients without direct exposure to pigs in a regional pork industry territory
- Fatal Case of Klebsiella Meningitis Combined with Bilateral Sudden Sensorineural Hearing Loss: A Case Report and Literature Review
- A Case of Streptococcus suis Infection Causing Pneumonia with Empyema in Korea