J Korean Med Sci.
2014 Mar;29(3):423-430. 10.3346/jkms.2014.29.3.423.
The Extended Rapid Response System: 1-Year Experience in a University Hospital
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Hanyang University Hospital, Seoul, Korea.
- 2Hanyang Rapid Response Team (HaRRT), Hanyang University Hospital, Seoul, Korea. mdoim@hanmail.net
- 3Division of Cardiology, Hanyang University Hospital, Seoul, Korea.
- 4Division of Nephrology and Department of Quality Improvement, Hanyang University Hospital, Seoul, Korea.
- 5The Hospital President Office of Hanyang University Hospital, Seoul, Korea.
- 6The Chief Executive Office of Hanyang University Medical Center, Seoul, Korea.
- KMID: 1734932
- DOI: http://doi.org/10.3346/jkms.2014.29.3.423
Abstract
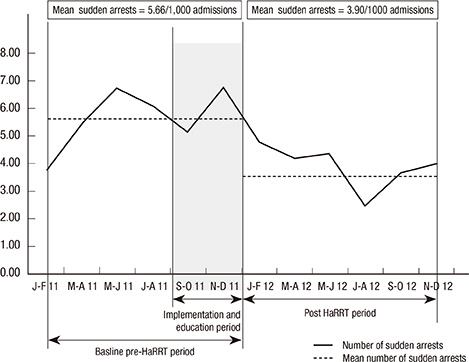
- The rapid response system (RRS) is an innovative system designed for in-hospital, at-risk patients but underutilization of the RRS generally results in unexpected cardiopulmonary arrests. We implemented an extended RRS (E-RRS) that was triggered by actively screening at-risk patients prior to calls from primary medical attendants. These patients were identified from laboratory data, emergency consults, and step-down units. A four-member rapid response team was assembled that included an ICU staff, and the team visited the patients more than twice per day for evaluation, triage, and treatment of the patients with evidence of acute physiological decline. The goal was to provide this treatment before the team received a call from the patient's primary physician. We sought to describe the effectiveness of the E-RRS at preventing sudden and unexpected arrests and in-hospital mortality. Over the 1-yr intervention period, 2,722 patients were screened by the E-RRS program from 28,661 admissions. There were a total of 1,996 E-RRS activations of simple consultations for invasive procedures. After E-RRS implementation, the mean hospital code rate decreased by 31.1% and the mean in-hospital mortality rate was reduced by 15.3%. In conclusion, the implementation of E-RRS is associated with a reduction in the in-hospital code and mortality rates.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Early Experience of Medical Alert System in a Rural Training Hospital: a Pilot Study
Maru Kim
Korean J Crit Care Med. 2017;32(1):47-51. doi: 10.4266/kjccm.2016.00598.Epidemiology and Clinical Characteristics of Rapid Response Team Activations
Sei Won Kim, Hwa Young Lee, Mi Ra Han, Yong Suk Lee, Eun Hyoung Kang, Eun Ju Jang, Keum Sook Jeun, Seok Chan Kim
Korean J Crit Care Med. 2017;32(2):124-132. doi: 10.4266/kjccm.2017.00199.Rapid response systems in Korea
Bo Young Lee, Sang-Bum Hong
Acute Crit Care. 2019;34(2):108-116. doi: 10.4266/acc.2019.00535.
Reference
-
1. Devita MA, Bellomo R, Hillman K, Kellum J, Rotondi A, Teres D, Auerbach A, Chen WJ, Duncan K, Kenward G, et al. Findings of the first consensus conference on medical emergency teams. Crit Care Med. 2006; 34:2463–2478.2. Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, Newhouse JP, Weiler PC, Hiatt HH. Harvard Medical Practice Study I. Incidence of adverse events and negligence in hospitalized patients: results of the Harvard Medical Practice Study I. 1991. Qual Saf Health Care. 2004; 13:145–151.3. Leape LL, Brennan TA, Laird N, Lawthers AG, Localio AR, Barnes BA, Hebert L, Newhouse JP, Weiler PC, Hiatt H. The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II. N Engl J Med. 1991; 324:377–384.4. Bell MB, Konrad D, Granath F, Ekbom A, Martling CR. Prevalence and sensitivity of MET-criteria in a Scandinavian University Hospital. Resuscitation. 2006; 70:66–73.5. Franklin C, Mathew J. Developing strategies to prevent inhospital cardiac arrest: analyzing responses of physicians and nurses in the hours before the event. Crit Care Med. 1994; 22:244–247.6. Schein RM, Hazday N, Pena M, Ruben BH, Sprung CL. Clinical antecedents to in-hospital cardiopulmonary arrest. Chest. 1990; 98:1388–1392.7. Bedell SE, Deitz DC, Leeman D, Delbanco TL. Incidence and character istics of preventable iatrogenic cardiac arrests. JAMA. 1991; 265:2815–2820.8. Smith AF, Wood J. Can some in-hospital cardio-respiratory arrests be prevented? a prospective survey. Resuscitation. 1998; 37:133–137.9. Buist MD, Jarmolowski E, Burton PR, Bernard SA, Waxman BP, Anderson J. Recognising clinical instability in hospital patients before cardiac arrest or unplanned admission to intensive care: a pilot study in a tertiary-care hospital. Med J Aust. 1999; 171:22–25.10. Hillman K, Bristow PJ, Chey T, Daffurn K, Jacques T, Norman SL, Bishop GF, Simmons G. Antecedents to hospital deaths. Intern Med J. 2001; 31:343–348.11. Naeem N, Montenegro H. Beyond the intensive care unit: a review of interventions aimed at anticipating and preventing in-hospital cardiopulmonary arrest. Resuscitation. 2005; 67:13–23.12. Jones DA, DeVita MA, Bellomo R. Rapid-response teams. N Engl J Med. 2011; 365:139–146.13. Baxter AD, Cardinal P, Hooper J, Patel R. Medical emergency teams at the Ottawa Hospital: the first two years. Can J Anaesth. 2008; 55:223–231.14. Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, Nguyen TV. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study. BMJ. 2002; 324:387–390.15. Shearer B, Marshall S, Buist MD, Finnigan M, Kitto S, Hore T, Sturgess T, Wilson S, Ramsay W. What stops hospital clinical staff from following protocols? an analysis of the incidence and factors behind the failure of bedside clinical staff to activate the rapid response system in a multi-campus Australian metropolitan healthcare service. BMJ Qual Saf. 2012; 21:569–575.16. Jones CM, Bleyer AJ, Petree B. Evolution of a rapid response system from voluntary to mandatory activation. Jt Comm J Qual Patient Saf. 2010; 36:266–270.17. Gerdik C, Vallish RO, Miles K, Godwin SA, Wludyka PS, Panni MK. Successful implementation of a family and patient activated rapid response team in an adult level 1 trauma center. Resuscitation. 2010; 81:1676–1681.18. Jones L, King L, Wilson C. A literature review: factors that impact on nurses’ effective use of the Medical Emergency Team (MET). J Clin Nurs. 2009; 18:3379–3390.19. Foraida MI, DeVita MA, Braithwaite RS, Stuart SA, Brooks MM, Simmons RL. Improving the utilization of medical crisis teams (Condition C) at an urban tertiary care hospital. J Crit Care. 2003; 18:87–94.20. Bellomo R, Goldsmith D, Uchino S, Buckmaster J, Hart G, Opdam H, Silvester W, Doolan L, Gutteridge G. Prospective controlled trial of effect of medical emergency team on postoperative morbidity and mortality rates. Crit Care Med. 2004; 32:916–921.21. Bellomo R, Goldsmith D, Uchino S, Buckmaster J, Hart GK, Opdam H, Silvester W, Doolan L, Gutteridge G. A prospective before-and-after trial of a medical emergency team. Med J Aust. 2003; 179:283–287.22. Downey AW, Quach JL, Haase M, Haase-Fielitz A, Jones D, Bellomo R. Characteristics and outcomes of patients receiving a medical emergency team review for acute change in conscious state or arrhythmias. Crit Care Med. 2008; 36:477–481.23. Chen J, Bellomo R, Flabouris A, Hillman K, Finfer S. MERIT Study Investigators for the Simpson Centre. ANZICS Clinical Trials Group. The relationship between early emergency team calls and serious adverse events. Crit Care Med. 2009; 37:148–153.24. Subbe C, Davies R, Williams E, Rutherford P, Gemmell L. Effect of introducing the Modified Early Warning score on clinical outcomes, cardio-pulmonary arrests and intensive care utilisation in acute medical admissions. Anaesthesia. 2003; 58:797–802.25. Duckitt RW, Buxton-Thomas R, Walker J, Cheek E, Bewick V, Venn R, Forni LG. Worthing physiological scoring system: derivation and validation of a physiological early-warning system for medical admissions: an observational, population-based single-centre study. Br J Anaesth. 2007; 98:769–774.26. Ravikumar TS, Sharma C, Marini C, Steele GD Jr, Ritter G, Barrera R, Kim M, Safyer SM, Vandervoort K, De Geronimo M, et al. A validated value-based model to improve hospital-wide perioperative outcomes: adaptability to combined medical/surgical inpatient cohorts. Ann Surg. 2010; 252:486–498.27. Hillman K, Chen J, Cretikos M, Bellomo R, Brown D, Doig G, Finfer S, Flabouris A. MERIT study investigators. Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. Lancet. 2005; 365:2091–2097.28. Jones D, Bellomo R, Bates S, Warrillow S, Goldsmith D, Hart G, Opdam H, Gutteridge G. Long term effect of a medical emergency team on cardiac arrests in a teaching hospital. Crit Care. 2005; 9:R808–R815.29. Buist M, Harrison J, Abaloz E, Van Dyke S. Six year audit of cardiac arrests and medical emergency team calls in an Australian outer metropolitan teaching hospital. BMJ. 2007; 335:1210–1212.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Influencing the Activation Time of the Rapid Response Team
- Effects of a Rapid Response Team on the Clinical Outcomes of Cardiopulmonary Resuscitation of Patients Hospitalized in General Wards
- Rapid response systems in Korea
- Strategies for successful implementation and permanent maintenance of a rapid response system
- Attention Circuits Mediate the Connection between Emotional Experience and Expression within the Emotional Circuit