Korean J Radiol.
2007 Oct;8(5):382-389. 10.3348/kjr.2007.8.5.382.
Breast MRI for Evaluating Patients with Metastatic Axillary Lymph Node and Initially Negative Mammography and Sonography
- Affiliations
-
- 1Department of Radiology and the Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. bkhan@smc.samsung.co.kr
- KMID: 1734286
- DOI: http://doi.org/10.3348/kjr.2007.8.5.382
Abstract
OBJECTIVE
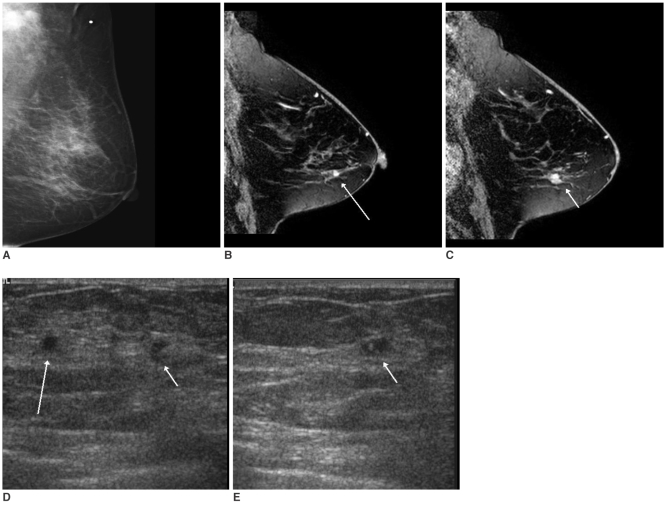
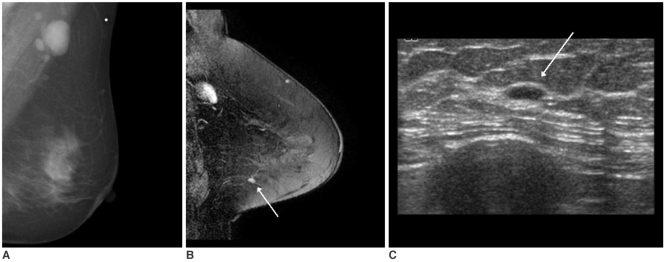
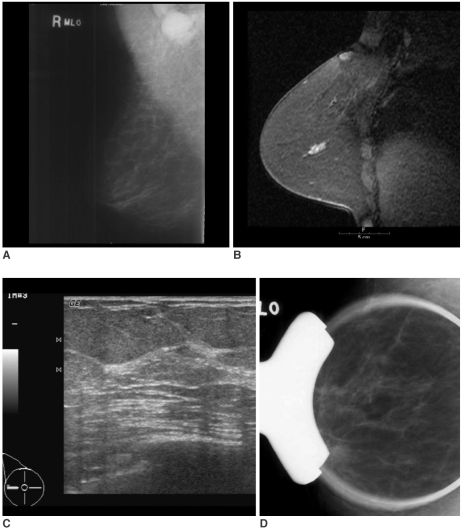
We wanted to investigate the ability of breast MR imaging to identify the primary malignancy in patients with axillary lymph node metastases and initially negative mammography and sonography, and we correlated those results with the conventional imaging. MATERIALS AND METHODS: From September 2001 to April 2006, 12 patients with axillary lymph node metastases and initially negative mammography and sonography underwent breast MR imaging to identify occult breast carcinoma. We analyzed the findings of the MR imaging, the MR-correlated mammography and the second-look sonography. We followed up both the MR-positive and MR-negative patients. RESULTS: MR imaging detected occult breast carcinoma in 10 of 12 (83%) patients. Two MR-negative patients were free of carcinoma in the ipsilateral breast during their follow-up period (39 and 44 months, respectively). In nine out of 10 patients, the MR-correlated mammography and second-look sonography localized lesions that were not detected on the initial exam. All the non-MR-correlated sonographic abnormalities were benign. CONCLUSION: Breast MR imaging can identify otherwise occult breast cancer in patients with metastatic axillary lymph nodes. Localization of the lesions through MR-correlated mammography and second-look sonography is practically feasible in most cases.
Keyword
MeSH Terms
-
Adenocarcinoma/*diagnosis
Adult
Aged
Axilla
Biopsy
Breast/pathology
Breast Neoplasms/*diagnosis/secondary
Contrast Media/administration & dosage
Feasibility Studies
Female
Follow-Up Studies
Gadolinium DTPA/diagnostic use
Humans
Image Processing, Computer-Assisted
Lymph Nodes/*pathology
Lymphatic Metastasis/diagnosis
Lymphoma, Large B-Cell, Diffuse/*diagnosis
Magnetic Resonance Imaging/*methods
Mammography/*methods
Middle Aged
Neoplasms, Unknown Primary/*diagnosis
Ultrasonography, Mammary/*methods
Figure
Cited by 1 articles
-
The Comparative Study of Ultrasonography, Contrast-Enhanced MRI, and 18F-FDG PET/CT for Detecting Axillary Lymph Node Metastasis in T1 Breast Cancer
Seung Ook Hwang, Sang-Woo Lee, Hye Jung Kim, Wan Wook Kim, Ho Yong Park, Jin Hyang Jung
J Breast Cancer. 2013;16(3):315-321. doi: 10.4048/jbc.2013.16.3.315.
Reference
-
1. Orel SG, Weinstein SP, Schnall MD, Reynolds CA, Schuchter LM, Fraker DL, et al. Breast MR imaging in patients with axillary node metastases and unknown primary malignancy. Radiology. 1999; 212:543–549. PMID: 10429716.
Article2. Ellerbroek N, Holmes F, Singletary E, Evans H, Oswald M, McNeese M. Treatment of patients with isolated axillary nodal metastases from an occult primary carcinoma consistent with breast origin. Cancer. 1990; 66:1461–1467. PMID: 2207996.
Article3. Jackson B, Scott-Conner C, Moulder J. Axillary metastasis from occult breast carcinoma: diagnosis and management. Am J Surg. 1995; 61:431–434.4. Kemeny MM, Rivera DE, Terz JJ, Benfield JR. Occult primary adenocarcinoma with axillary metastases. Am J Surg. 1986; 152:43–47. PMID: 3728816.
Article5. Orel SG, Schnall MD. MR imaging of the breast for the detection, diagnosis, and staging of breast cancer. Radiology. 2001; 220:13–30. PMID: 11425968.
Article6. American College of Radiology. BI-RADS: Breast Imaging Reporting and Data System Atlas(BI-RADS®) atlas. 2003. 4th ed. Reston: American College of Radiology.7. Harvey JA, Fajardo LL, Innis CA. Previous mammograms in patients with impalpable breast carcinoma: retrospective vs blinded interpretation. 1993 ARRS President's Award. AJR Am J Roentgenol. 1993; 161:1167–1172. PMID: 8249720.
Article8. Majid AS, de Paredes ES, Doherty RD, Sharma NR, Salvador X. Missed breast carcinoma: pitfalls and pearls. Radiographics. 2003; 23:881–895. PMID: 12853663.
Article9. Berg WA, Gutierrez L, NessAiver MS, Carter WB, Bhargavan M, Lewis RS, et al. Diagnostic accuracy of mammography, clinical examination, US, and MR imaging in preoperative assessment of breast cancer. Radiology. 2004; 233:830–849. PMID: 15486214.
Article10. Dershaw DD. Morris EA, Liberman L, editors. Magnetic resonance imaging as a clinical tool. Breast MRI; Diagnosis and intervention. 2004. New York, NY: Springer;p. 256–264.
Article11. Obdeijn IM, Brouwers-Kuyper EM, Tilanus-Linthorst MM, Wiggers T, Oudkerk M. MR imaging-guided sonography followed by fine-needle aspiration cytology in occult carcinoma of the breast. AJR Am J Roentgenol. 2000; 174:1079–1084. PMID: 10749254.
Article12. Morris EA, Schwartz LH, Dershaw DD, van Zee KJ, Abramson AF, Liberman L. MR imaging of the breast in patients with occult primary breast carcinoma. Radiology. 1997; 205:437–440. PMID: 9356625.
Article13. Schorn C, Fischer U, Luftner-Nagel S, Westerhof JP, Grabbe E. MRI of the breast in patients with metastatic disease of unknown primary. Eur Radiol. 1999; 9:470–473. PMID: 10087118.
Article14. Kuhl CK, Morakkabati N, Leutner CC, Schmiedel A, Wardelmann E, Schild HH. MR imaging-guided large-core (14-gauge) needle biopsy of small lesions visible at breast MR imaging alone. Radiology. 2001; 220:31–39. PMID: 11425969.
Article15. Zujewski J, Eng-Wong J. Sentinel lymph node biopsy in the management of ductal carcinoma in situ. Clin Breast Cancer. 2005; 6:216–222. PMID: 16137431.
Article16. Sakr R, Barranger E, Antoine M, Prugnolle H, Daraï E, Uzan S. Ductal carcinoma in situ: value of sentinel lymph node biopsy. J Surg Oncol. 2006; 94:426–430. PMID: 16967457.
Article17. Lara JF, Young SM, Velilla RE, Santoro EJ, Templeton SF. The relevance of occult axillary micrometastasis in ductal carcinoma in situ: a clinicopathologic study with long-term follow-up. Cancer. 2003; 98:2105–2113. PMID: 14601079.18. Harms SE, Flamig DP, Hesley KL, Meiches MD, Jensen RA, Evans WP, et al. MR imaging of the breast with rotating delivery of excitation off resonance: clinical experience with pathologic correlation. Radiology. 1993; 187:493–501. PMID: 8475297.
Article19. Friedman P, Sanders L, Russo J, Sharo R, Swaminathan S, Smith R. Detection and localization of occult lesions using breast magnetic resonance imaging: initial experience in a community hospital. Acad Radiol. 2005; 12:728–738. PMID: 15935971.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasonography for Staging Axillary Lymph Node in Breast Cancer Patients
- Efficacy of Ultrasound-Guided Core Needle Biopsy in Detecting Metastatic Axillary Lymph Nodes in Breast Cancer
- The Role of Sonography in Patients with Breast Cancer Presenting as an Axillary Mass
- Carcinoma of the Axillary Tail of Spence: A Case Report with Imaging Findings
- The Accuracy of the Physical Examination, Mammography, and Ultrasonography in the Assessment of Tumor Size and Axillary Lymph Node Metastasis in Breast Cancer Patient