Korean J Radiol.
2008 Feb;9(1):87-90. 10.3348/kjr.2008.9.1.87.
Pulmonary Paraganglioma Manifesting as an Endobronchial Mass
- Affiliations
-
- 1Department of Radiology, College of Medicine, Dong-A University, Pusan, Korea. gnlee@dau.ac.kr
- 2Department of Pathology, College of Medicine, Dong-A University, Pusan, Korea.
- 3Department of Thoracic and Cardiovascular Surgery, College of Medicine, Dong-A University, Pusan, Korea.
- 4Internal Medicine, College of Medicine, Dong-A University, Pusan, Korea.
- KMID: 1734281
- DOI: http://doi.org/10.3348/kjr.2008.9.1.87
Abstract
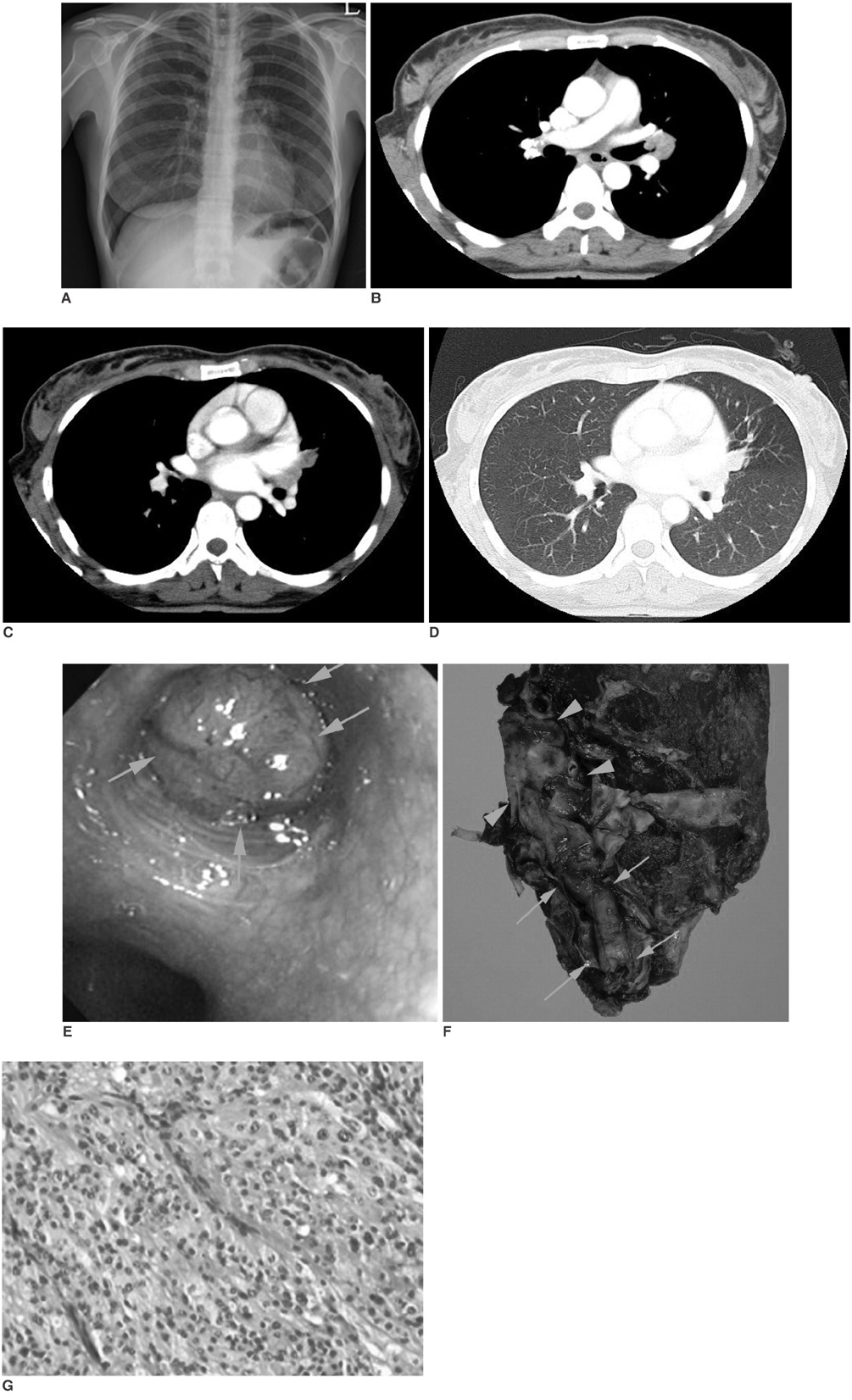
- Thoracic paragangliomas comprise only 1-2% of all paragangliomas, including the adrenal pheochromocytomas, and these tumors are mostly found in the mediastinal compartments (1). To the best of our knowledge, there is only one case report in the pathology literature of endobronchial involvement by a primary pulmonary paraganglioma (2). We report here on the CT and bronchoscopic findings of a case of pathologically proven endobronchial paraganglioma in a 37-year-old woman. In our case, bronchoscopy and CT demonstrated an endobronchial hypervascular mass, which indicated the presence of carcinoid or hypervascular metastasis based on the known incidence of such tumors.
Keyword
MeSH Terms
Figure
Reference
-
1. Aravot DJ, Banner NR, Cantor AM, Theodoropoulos S, Yacoub MH. Location, localization and surgical treatment of cardiac pheochromocytoma. Am J Cardiol. 1992. 69:283–285.2. Aubertine CL, Flieder DB. Primary paraganglioma of the lung. Ann Diagn Pathol. 2004. 8:237–241.3. Rosai J. Ackerman's surgical pathology. 1996. 8th ed. New York: Mosby;1015–1058.4. Saeki T, Akiba T, Joh K, Inoue K, Doi N, Kanai M, et al. An extremely large solitary primary paraganglioma of the lung: report of a case. Surg Today. 1999. 29:1195–1200.5. Sandur S, Dasgupta A, Shapiro JL, Arroliga AC, Mehta AC. Thoracic involvement with pheochromocytoma: a review. Chest. 1999. 115:511–521.6. Whalen RK, Althausen AF, Daniels GH. Extra-adrenal pheochromocytoma. J Urol. 1992. 147:1–10.7. Linnoila RI, Keiser HR, Steinberg SM, Lack EE. Histopathology of benign versus malignant sympathoadrenal paragangliomas: clinicopathologic study of 120 cases including unusual histologic features. Hum Pathol. 1990. 21:1168–1180.8. Lemonick DM, Pai PB, Hines GL. Malignant primary pulmonary paragagnlioma with hilar metastasis. J Thorac Cardiovasc Surg. 1990. 99:563–564.9. Hangartner JR, Loosemore TM, Burke M, Pepper JR. Malignant primary pulmonary paraganglioma. Thorax. 1989. 44:154–156.10. Fenandez-Llamazares J, Sabria-Leal M, Armengol-Carrasco M, Garsia-Bonafe M, Salca-Lacombe JA. Functioning metastases of a nonfunctioning paraganglioma. J Surg Oncol. 1988. 37:213–214.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Treatment for Primary Pulmonary Paraganglioma : A case report
- A Case of Pulmonary Mucormycosis Presenting as an Endobronchial Mass
- Functioning Paraganglioma Manifested Cerebral Hemorrhage and Combined with Coronary Arterio-Venous Fistula
- Paraganglioma of the Cauda Equina: Case Report
- A Case of Nonfunctional Paraganglioma of Retroperitonium