Ewha Med J.
2013 Dec;36(Suppl):S9-S13. 10.12771/emj.2013.36.S.S9.
Acute Pancreatitis Associated with Intraductal Tubulopapillary Neoplasm of the Pancreas
- Affiliations
-
- 1Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 2Division of Gastroenterology, Department of Internal Medicine, Changwon Fatima Hospital, Changwon, Korea. jyhyhj@chol.com
- 3Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 1726727
- DOI: http://doi.org/10.12771/emj.2013.36.S.S9
Abstract
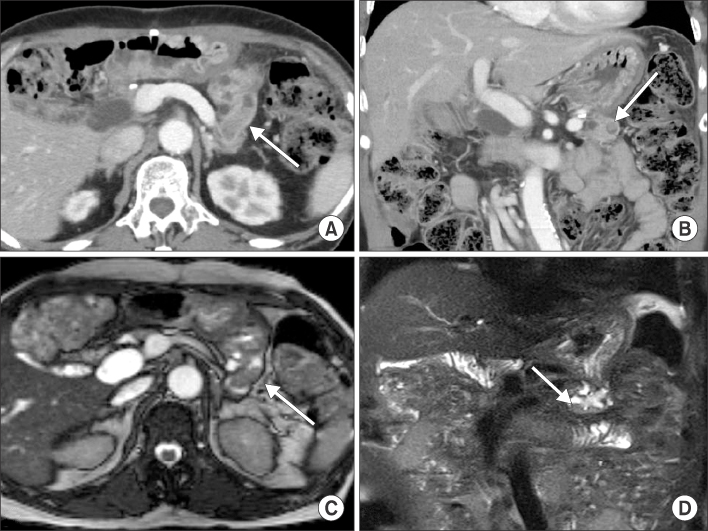
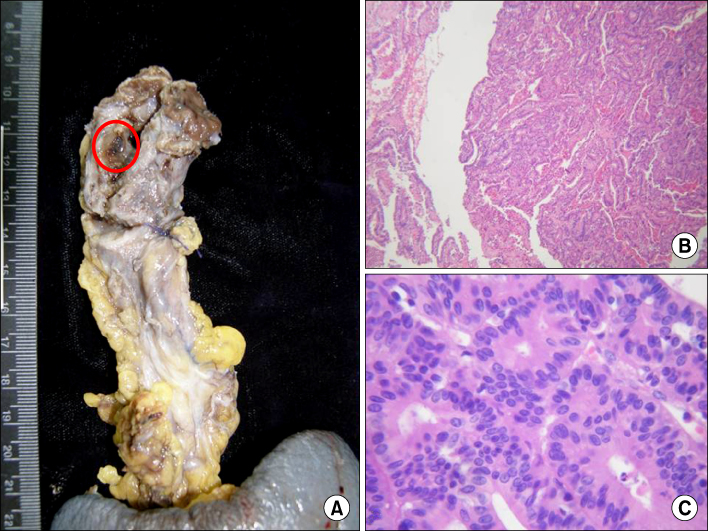
- Intraductal tubulopapillary neoplasm (ITPN) of the pancreas has been recently reported. It is very rare, therefore clinical behavior and prognosis has not yet been characterized. We experienced a case of ITPN of the pancreas which presented with acute pancreatitis and treated with Whipple's operation. Histopathologic finding showed papillary hyperplasia with carcinomatous change. The tumor recurred after 47 month of operation, and she underwent total pancreatectomy. Pathologic finding revealed tubulopapillary growth with high grade dysplasia. Immunohistochemial staining was not performed, however gross and microscopic findings were compatible with ITPN of the pancreas. We report a case of ITPN of the pancreas.
Figure
Reference
-
1. Yamaguchi H, Shimizu M, Ban S, Koyama I, Hatori T, Fujita I, et al. Intraductal tubulopapillary neoplasms of the pancreas distinct from pancreatic intraepithelial neoplasia and intraductal papillary mucinous neoplasms. Am J Surg Pathol. 2009; 33:1164–1172.2. Longnecker DS, Adler G, Hruban RH, Kloppel G. Intraductal papillary-mucinous neoplasms of the pancreas. In : Hamilton SR, Aaltonen LA, editors. Pathology and genetics of tumours of the digestive system WHO classification of tumours. Lyon, France: IARC Press;2000. p. 237–240.3. Bosman FT, Carneiro F, Hruban RH, Theise ND. WHO classification of tumours of the digestive system. 2nd ed. Lyon, France: IARC Press;2010.4. Bhuva N, Wasan H, Spalding D, Stamp G, Harrison M. Intraductal tubulopapillary neoplasm of the pancreas as a radiation induced malignancy. BMJ Case Rep. 2011; 2011:pii: bcr0920114777. 10.1136/bcr.09.2011.4777.5. Guan H, Gurda G, Marie Lennon A, Hruban RH, Erozan YS. Intraductal tubulopapillary neoplasm of the pancreas on fine needle aspiration: case report with differential diagnosis. Diagn Cytopathol. 2012; 07. 16. [Epub]. 10.1002/dc.22890.6. Jokoji R, Tsuji H, Tsujimoto M, Shinno N, Tori M. Intraductal tubulopapillary neoplasm of pancreas with stromal osseous and cartilaginous metaplasia; a case report. Pathol Int. 2012; 62:339–343.7. Tajiri T, Tate G, Matsumoto K, Hoshino H, Iwamura T, Kodaira Y, et al. Diagnostic challenge: intraductalneoplasms of the pancreatobiliary system. Pathol Res Pract. 2012; 208:691–696.8. Hruban RH, Adsay NV, Albores-Saavedra J, Compton C, Garrett ES, Goodman SN, et al. Pancreatic intraepithelial neoplasia: a new nomenclature and classification system for pancreatic duct lesions. Am J Surg Pathol. 2001; 25:579–586.9. Furukawa T, Kloppel G, Volkan Adsay N, Albores-Saavedra J, Fukushima N, Horii A, et al. Classification of types of intraductal papillary-mucinous neoplasm of the pancreas: a consensus study. Virchows Arch. 2005; 447:794–799.10. Tajiri T, Tate G, Inagaki T, Kunimura T, Inoue K, Mitsuya T, et al. Intraductal tubular neoplasms of the pancreas: histogenesis and differentiation. Pancreas. 2005; 30:115–121.11. Park HJ, Jang KT, Heo JS, Choi YL, Han J, Kim SH. A potential case of intraductal tubulopapillary neoplasms of the bile duct. Pathol Int. 2010; 60:630–635.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Branch Duct Intraductal Papillary Mucinous Neoplasm Mimicking Pseudocysts Complicated by Recurrent Pancreatitis
- Intraductal Papillary Mucinous Neoplasm with an Associated Invasive Carcinoma Manifested by Acute Pancreatitis
- Intraductal tubulopapillary neoplasms of the pancreas and biliary tract: The black swan of hepatobiliary surgery
- Differential diagnosis of cystic diseases of pancreas
- Acute Pancreatitis Associated with Diaphragmatic Hernia in an Adult