Tuberc Respir Dis.
2006 Apr;60(4):379-390. 10.4046/trd.2006.60.4.379.
Immunopathogenesis of Asthma
- Affiliations
-
- 1Division of Respiratory and Critical Care Medicine, Department of Internal Medicine, College of Medicine, Korea University Anam Hospital, Seoul, Korea. khin@kumc.or.kr
- KMID: 1719362
- DOI: http://doi.org/10.4046/trd.2006.60.4.379
Abstract
- No abstract available.
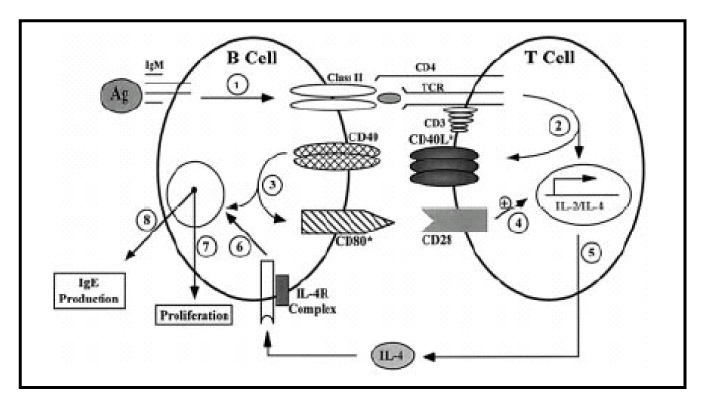
MeSH Terms
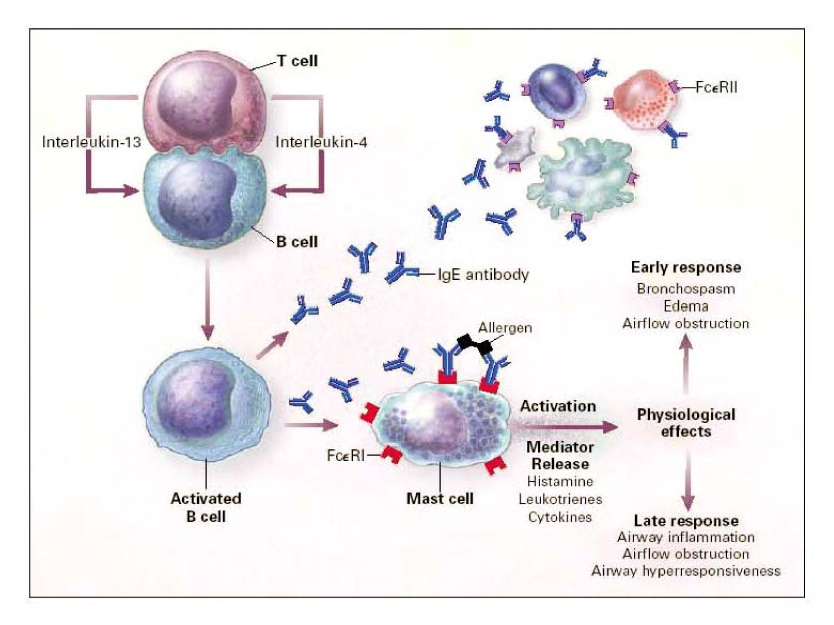
Figure
Reference
-
1. Busse WW, Lemanske RF Jr. Asthma. N Engl J Med. 2001. 344:350–362.2. Haley KJ, Sunday ME, Wiggs BR, et al. Inflammatory cell distribution within and along asthmatic airways. Am J Respir Crit Care Med. 1998. 158:565–572.3. Kraft M, Djukanovic R, Wilson S, Holgate ST, Martin RJ. Alveolar tissue inflammation in asthma. Am J Respir Crit Care Med. 1996. 154:1505–1510.4. Vignola AM, Chanez P, Campbell AM, et al. Airway inflammation in mild intermittent and in persistent asthma. Am J Respir Crit Care Med. 1998. 157:403–409.5. Burrows B, Martinez FD, Halonen M, Barbee RA, Cline MG. Association of asthma with serum IgE levels and skin-test reactivity to allergens. N Engl J Med. 1989. 320:271–277.6. Noah TL, Becker S. Chemokines in nasal secretions of normal adults experimentally infected with respiratory syncytial virus. Clin Immunol. 2000. 97:43–49.7. Schwartz RS. A new element in the mechanism of asthma. N Engl J Med. 2002. 346:857–858.8. National Asthma Education and Prevention Program. Guidelines for the diagnosis and management of asthma. 2004. Bethesda, MD: National Heart, Lung, and Blood Institute, National Institutes of Health.9. Wills-Karp M, Luyimbazi J, Xu X, et al. Interleukin-13: central mediator of allergic asthma. Science. 1998. 282:2258–2261.10. Bacharier LB, Jabara H, Geha RS. Molecular mechanisms of immunoglobulin E regulation. Int Arch Allergy Immunol. 1998. 115:257–269.11. Siraganian RP. Middleton E, Reed CE, Ellis EF, Adkinson NF, Yunginger JW, Busse WW, editors. Biochemical events in basophil or mast cell activation and mediator release. Allergy: principles & practice. 1998. Vol. 1:5th ed. St. Louis: Mosby-Year Book;204–227.12. Galli SJ. Complexity and redundancy in the pathogenesis of asthma: reassessing the roles of mast cells and T cells. J Exp Med. 1997. 186:343–347.13. Lane SJ, Lee TH. Mast cell effector mechanisms. J Allergy Clin Immunol. 1996. 98:S67–S72.14. Clark JM, Abraham WM, Fishman CE, et al. Tryptase inhibitors block allergen-induced airway and inflammatory responses in allergic sheep. Am J Respir Crit Care Med. 1995. 152:2076–2083.15. Brandenburg AH, van Beek R, Moll HA, Osterhaus ADME, Claas ECJ. G protein variation in respiratory syncytial virus group A does not correlate with clinical severity. J Clin Microbiol. 2000. 38:3849–3852.16. Peters SP, Zangrilli JG, Fish JE. Middleton E, Reed CE, Ellis EF, Adkinson NF, Yunginger JW, Busse WW, editors. Late phase allergic reactions. Allergy: principles & practice. 1998. Vol. 1:5th ed. St. Louis: Mosby-Year Book;342–355.17. Sanderson CJ. Interleukin-5, eosinophils, and disease. Blood. 1992. 79:3101–3109.18. Rothenberg ME. Eosinophilia. N Engl J Med. 1998. 338:1592–1600.19. Bochner BS. Cellular adhesion and its antagonism. J Allergy Clin Immunol. 1997. 100:581–585.20. Wardlaw AJ. Molecular basis for selective eosinophil trafficking in asthma: a multistep paradigm. J Allergy Clin Immunol. 1999. 104:917–926.21. Nagata M, Sedgwick JB, Bates ME, Kita H, Busse WW. Eosinophil adhesion to vascular cell adhesion molecule-1 activates superoxide anion generation. J Immunol. 1995. 155:2194–2202.22. Yamamoto H, Sedgwick JB, Busse WW. Differential regulation of eosinophil adhesion and transmigration by pulmonary microvascular endothelial cells. J Immunol. 1998. 161:971–977.23. Hamid QA, Minshall EM. Molecular pathology of allergic disease. I. Lower airway disease. J Allergy Clin Immunol. 2000. 105:20–36.24. Nakamura Y, Ghaffar O, Olivenstein R, et al. Gene expression of the GATA-3 transcription factor is increased in atopic asthma. J Allergy Clin Immunol. 1999. 103:215–222.25. Robinson DS, Hamid Q, Ying S, et al. Predominant TH2-like bronchoalveolar T-lymphocyte population in atopic asthma. N Engl J Med. 1992. 326:298–304.26. Walker C, Bauer W, Braun RK, et al. Activated T cells and cytokines in bronchoalveolar lavages from patients with various lung diseases associated with eosinophilia. Am J Respir Crit Care Med. 1994. 150:1038–1048.27. Aubus P, Cosso B, Godard P, et al. Decreased suppressor cell activity of alveolar macrophages in bronchial asthma. Am Rev Respir Dis. 1984. 130:875–878.28. Spiteri M, Knight RA, Jeremy JY, et al. Alveolar macrophage-induced suppression of T-cell hyperresponsiveness in bronchial asthma is reversed by allergen exposure. Eur Respir J. 1994. 7:1431–1438.29. Chung KF, Barnes PJ. Cytokines in asthma. Thorax. 1999. 54:825–857.30. Brewster CEP, Howarth PH, Djukanovic R, et al. Myofibroblasts and subepithelial fibrosis in bronchial asthma. Am J Respir Cell Mol Biol. 1990. 3:507–511.31. Hirst SJ, Barnes PJ, Twort CHL. Quantifying proliferation of cultured human and rabbit airway smooth muscle cells in response to serum and platelet-derived growth factor. Am J Respir Cell Mol Biol. 1992. 7:574–581.32. Cerutis DR, Nogami M, Anderson JL, et al. Lysophosphatidic acid and EGF stimulate mitogenesis in human airway smooth muscle cells. Am J Physiol. 1997. 273:L10–L15.33. Lynch KR, O'Neil GP, Liu Q, et al. Characterization of the human cysteinyl leukotriene CysLT1 receptor. Nature. 1999. 399:789–793.34. Yokomizo T, Izumi T, Chang K, et al. A G-protein-coupled receptor for leukotriene B4 that mediates chemotaxis. Nature. 1997. 387:620–624.35. Stafforini DM, Satoh K, Atkinson DL, et al. Platelet-activating factor acetylhydrolase deficiency : a missense mutation near the active site of an anti-inflammatory phospholipase. J Clin Invest. 1996. 97:2784–2791.36. Stafforini DM, Numao T, Tsodikov A, et al. Deficiency of platelet-activating factor acetylhydrolase is a severity factor for asthma. J Clin Invest. 1999. 103:989–997.37. Levitt RC, McLane MP, MacDonald D, et al. IL-9 pathway in asthma: new therapeutic targets for allergic inflammatory disorders. J allergy Clin Immunol. 1999. 103:S485–S491.38. Holroyd KJ, Martinati LC, Trabetti E, et al. Asthma and bronchial hyperresponsiveness linked to the XY long arm pseudoautosomal region. Genomics. 1998. 52:233–235.39. McLane MP, Haczku A, van de Rijn M, et al. Interleukin-9 promotes allergen-induced eosinophilic inflammation and airway hyperresponsiveness in transgenic mice. Am J Respir Cell Mol Biol. 1998. 19:713–720.40. Humbles AA, Lu B, Nilsson CA, et al. A role for the C3a anaphylatoxin receptor in the effector phase of asthma. Nature. 2000. 161:998–1001.41. Karp CL, Grupe A, Schadt E, et al. Identification of complement factor 5 as a susceptibility locus for experimental allergic asthma. Nat Immunol. 2000. 1:221–226.42. Chalmers GW, Thomson L, Macleod KJ, et al. Endothelin-1 levels in induced sputum samples from asthmatic and normal subjects. Thorax. 1997. 100:544–552.43. Redington AE, Springall DR, Ghatei MA, et al. Airway endothelin levels in asthma: influence of endobronchial allergen challenge and maintenance corticosteroid therapy. Eur Respir J. 1997. 10:1026–1032.44. Redington AE, Springall DR, Meng QH, et al. Immunoreactive endothelin in bronchial biopsy specimens: increased expression in asthma and modulation by corticosteroid therapy. J Allergy Clin Immunol. 1997. 100:544–552.45. Gustafsson LE, Leone AM, Persson MG, Wiklund NP, Moncada S. Endogenous nitric oxide is present in the exhaled air of rabbits, guinea pigs and humans. Biochem Biophys Res Commun. 1991. 181:852–857.46. Kharitonov SA, Yates D, Robbins RA, et al. Increased nitric oxide in exhaled air of asthmatic patients. Lancet. 1994. 343:133–135.47. Massaro AF, Mehta S, Lilly CM, et al. Elevated nitric oxide concentrations in isolated lower airway gas of asthmatic subjects. Am J Respir Crit Care Med. 1996. 153:1510–1514.48. Jatakanon A, Lim S, Kharitonov SA, Chung KF, Barnes PJ. Correlation between exhaled nitric oxide, sputum eosinophils, and methacholine responsiveness in patients with mild asthma. Thorax. 1998. 53:91–95.49. Saleh D, Ernst P, Lim S, Barnes PJ, Giaid A. Increased formation of the potent oxidant peroxynitrite in the airways of asthmatic patients is associated with induction of nitric oxide synthase: effect of inhaled glucocorticoid. FASEB J. 1998. 12:929–937.50. Barnes PJ, Karin M. Nuclear factor-kappaB: a pivotal transcription factor in chronic inflammatory diseases. N Engl J Med. 1997. 336:1066–1071.51. Hart LA, Krishnan VL, Adcock IM, Barnes PJ, Chung KF. Activation and localization of transcription factor, nuclear factor-kappaB, in asthma. Am J Respir Crit Care Med. 1998. 158:1585–1592.52. Selig W, Tocker J. Effect of interleukin-1 receptor antagonist on antigen-induced pulmonary responses in guinea pigs. Eur J Pharmacol. 1992. 213:331–336.53. Naseer T, Minshall EM, Leung DY, et al. Expression of IL-12 and IL-13 mRNA in asthma and their modulation in response to steroid therapy. Am J Respir Crit Care Med. 1997. 155:845–851.54. Ho AS, Moore KW. Interleukin-10 and its receptor. Ther Immunol. 1994. 1:173–185.55. Wang P, Wu P, Siegel MI, Egan RW, Billah MM. Interleukin (IL)-10 inhibits nuclear factor kappa B (NF kappa B) activation in human monocytes. IL-10 and IL-4 suppress cytokine synthesis by different mechanisms. J Biol Chem. 1995. 270:9558–9563.56. Borish L, Aarons A, Rumbyrt J, et al. Interleukin-10 regulation in normal subjects and patients with asthma. J Allergy Clin Immunol. 1996. 97:1288–1296.57. John M, Lim S, Seybold J, et al. Inhaled corticosteroids increase interleukin-10 but reduce macrophage inflammatory protein-1alpha, granulocyte-macrophage colony-stimulating factor, and interferon-gamma release from alveolar macrophages in asthma. Am J Respir Crit Care Med. 1998. 157:256–262.58. Spiteri MA, Knight RA, Jeremy JY, et al. Alveolar macrophage-induced suppression of peripheral blood mononuclear cell responsiveness is reversed by in vitro allergen exposure in bronchial asthma. Eur Respir J. 1994. 7:1431–1438.59. Medzhitov R, Janeway C Jr. Innate immunity. N Engl J Med. 2000. 343:338–344.60. Eisenbarth SC, Classel S, Bottomly K. Understanding asthma pathogenesis: linking innate and adaptive immunity. Current opinion in Pediatrics. 2004. 16:659–665.61. Cembrzynska-Nowak M, Szklarz E, Inglot AD, Teodorczyk-Injeyan JA. Elevate release of tumor necrosis factor-α and interferon-γ by bron-choalveolar leukocytes from patients with bronchial asthma. Am Rev Respir Dis. 1993. 147:291–295.62. Krug N, Madden J, Redington AE, Lackie P, Djukanovic R, Schauer U, Holgate ST, Frew AJ, Howarth PH. T-cell cytokine profile evaluated at the single cell level in BAL and blood in allergic asthma. Am J Respir Cell Mol Biol. 1996. 14:319–326.63. Redecke V, Hacker H, Datta SK, et al. : Cutting edge: activation of Toll-like receptor 2 induces a Th2 immune response and promotes experimental asthma. J Immunol. 2004. 172:2739–2743.64. Walter MJ, Holtzman MJ. A centennial history of research on asthma pathogenesis. Am J Respir Cell Mol Biol. 2005. 32:483–489.