Clin Orthop Surg.
2010 Jun;2(2):69-75. 10.4055/cios.2010.2.2.69.
Factors Affecting Patients' Graft Choice in Anterior Cruciate Ligament Reconstruction
- Affiliations
-
- 1Department of Orthopaedic Surgery, Uijeongbu St. Mary's Hospital, The Catholic University of Korea School of Medicine, Uijeongbu, Korea. iy1000@catholic.ac.kr
- KMID: 1719332
- DOI: http://doi.org/10.4055/cios.2010.2.2.69
Abstract
- BACKGROUND
Multiple studies have reported that allografts are acceptable alternatives to autografts for anterior cruciate ligament (ACL) reconstructions. Our clinical practice allows patient involvement in graft decision-making. This study examined the patients' preference for graft selection and the factors affecting their decision.
METHODS
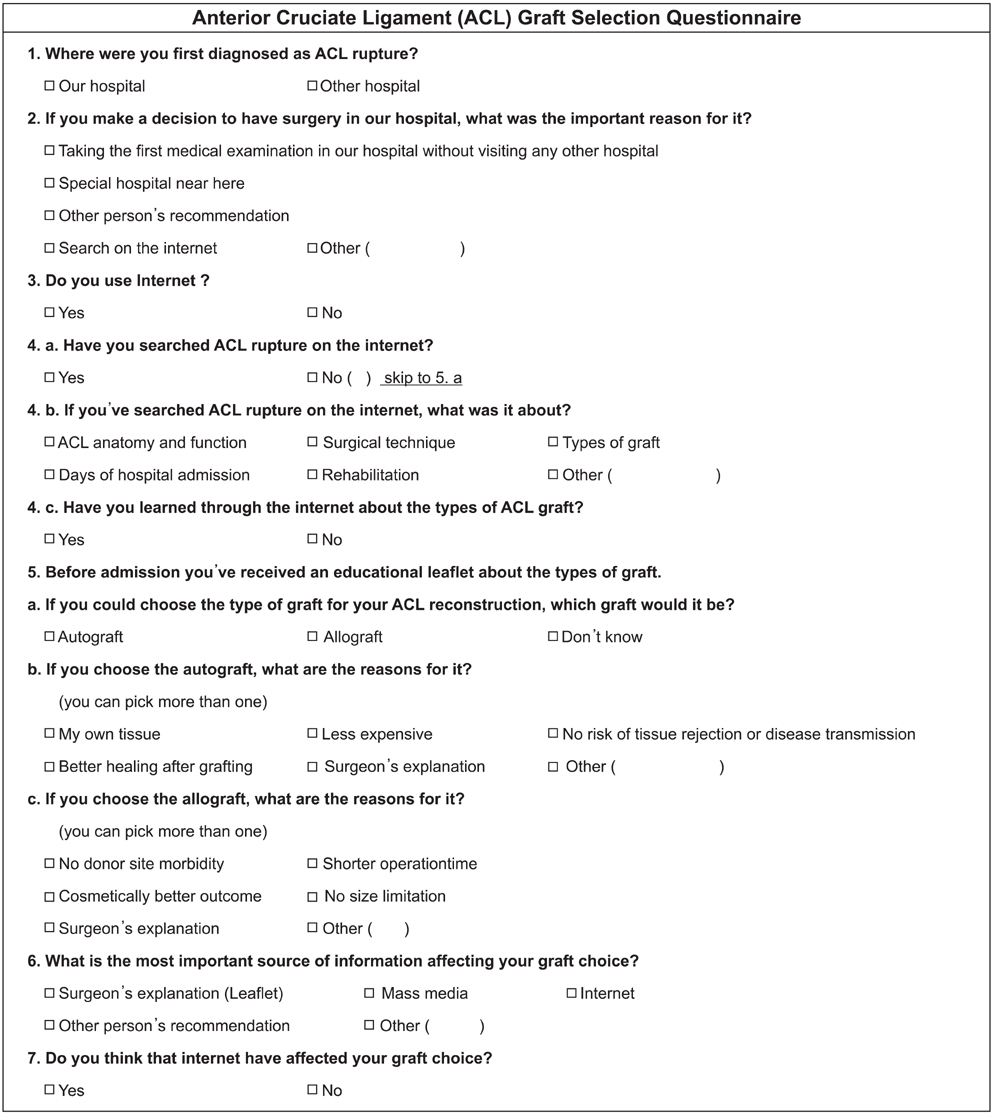
Patients scheduled to undergo an ACL reconstruction surgery (n = 129) at a university medical center in Korea were enrolled in this study. Information leaflets with graft descriptions were provided prior to hospital admission, and the patients were allowed to choose one of two surgical graft types. The patients were asked to complete a questionnaire that reflected their decision-making processes, and the patients' trends and factors affecting their choice of graft were analyzed based on their responses.
RESULTS
Most patients (54.3%) selected autografts for the ACL reconstruction. The surgeon's explanation was the most important factor affecting the final patient decision followed by the information derived from Internet searches. Patients who derived the majority of their understanding of the graft types from the Internet chose allografts at significantly higher rates.
CONCLUSIONS
Patient graft selection is a reasonable way of designating the type of surgical procedure. Most patients selected autografts for their ACL reconstruction. However, patients who performed significant Internet-based research tended to prefer allografts.
MeSH Terms
Figure
Reference
-
1. Sherman OH, Banffy MB. Anterior cruciate ligament reconstruction: which graft is best? Arthroscopy. 2004. 20(9):974–980.
Article2. Eriksson E. Auto- or allograft for ACL-reconstruction? Knee Surg Sports Traumatol Arthrosc. 2007. 15(6):689.
Article3. Barber FA. Should allografts be used for routine anterior cruciate ligament reconstructions? Arthroscopy. 2003. 19(4):421.
Article4. Salmon LJ, Russell VJ, Refshauge K, et al. Long-term outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft: minimum 13-year review. Am J Sports Med. 2006. 34(5):721–732.
Article5. Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007. 35(4):564–574.
Article6. Marrale J, Morrissey MC, Haddad FS. A literature review of autograft and allograft anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2007. 15(6):690–704.
Article7. Krych AJ, Jackson JD, Hoskin TL, Dahm DL. A meta-analysis of patellar tendon autograft versus patellar tendon allograft in anterior cruciate ligament reconstruction. Arthroscopy. 2008. 24(3):292–298.
Article8. West RV, Harner CD. Graft selection in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2005. 13(3):197–207.
Article9. Lebel B, Hulet C, Galaud B, Burdin G, Locker B, Vielpeau C. Arthroscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone autograft: a minimum 10-year follow-up. Am J Sports Med. 2008. 36(7):1275–1282.
Article10. Mauro CS, Irrgang JJ, Williams BA, Harner CD. Loss of extension following anterior cruciate ligament reconstruction: analysis of incidence and etiology using IKDC criteria. Arthroscopy. 2008. 24(2):146–153.
Article11. Breitfuss H, Frohlich R, Povacz P, Resch H, Wicker A. The tendon defect after anterior cruciate ligament reconstruction using the midthird patellar tendon: a problem for the patellofemoral joint? Knee Surg Sports Traumatol Arthrosc. 1996. 3(4):194–198.
Article12. Aune AK, Holm I, Risberg MA, Jensen HK, Steen H. Four-strand hamstring tendon autograft compared with patellar tendon-bone autograft for anterior cruciate ligament reconstruction: a randomized study with two-year follow-up. Am J Sports Med. 2001. 29(6):722–728.
Article13. Kassirer JP. Incorporating patients' preferences into medical decisions. N Engl J Med. 1994. 330(26):1895–1896.
Article14. Akerkar SM, Bichile LS. Doctor patient relationship: changing dynamics in the information age. J Postgrad Med. 2004. 50(2):120–122.15. Gerber BS, Eiser AR. The patient physician relationship in the Internet age: future prospects and the research agenda. J Med Internet Res. 2001. 3(2):E15.16. Eysenbach G, Diepgen TL. Towards quality management of medical information on the internet: evaluation, labelling, and filtering of information. BMJ. 1998. 317(7171):1496–1500.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Graft considerations for successful anterior cruciate ligament reconstruction
- Ligament Reconstruction in Congenital Absence of the Anterior Cruciate Ligament: A Case Report
- Graft Selection and Fixation in Anterior Cruciate Ligament Reconstruction
- Current Trends in Anterior Cruciate Ligament Reconstruction
- Anterior Cruciate Ligament Reconstruction with Achilles Tendon Allograft