Clin Orthop Surg.
2010 Dec;2(4):237-243. 10.4055/cios.2010.2.4.237.
Reliability of MRI Findings of Peroneal Tendinopathy in Patients with Lateral Chronic Ankle Instability
- Affiliations
-
- 1Department of Radiology, Myongji Hospital, Kwandong University College of Medicine, Goyang, Korea.
- 2Department of Orthopedic Surgery, Myongji Hospital, Kwandong University College of Medicine, Goyang, Korea. bladeplate@hanmail.net
- KMID: 1719325
- DOI: http://doi.org/10.4055/cios.2010.2.4.237
Abstract
- BACKGROUND
Patients with chronic lateral ankle instability also have peroneal tendinopathy often. However, preoperative MRIs of these patients are vague in many cases. Our study was performed to see the reliability of MRI findings of peroneal tendinopathy in patients with chronic lateral ankle instability.
METHODS
MRI images for 82 patients who had chronic lateral ankle instability, and had received surgical treatment between March 2006 and November 2009 were compared with impressions from operating rooms. The mean age of patients was 36.4 years (range, 15 to 64 years), 82 ankles were studied, and patients with rheumatoid diseases were excluded from the study.
RESULTS
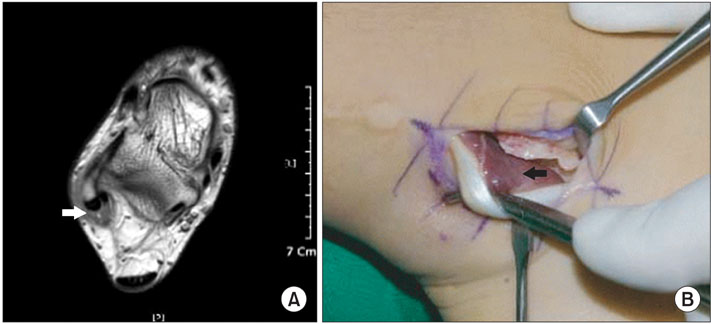
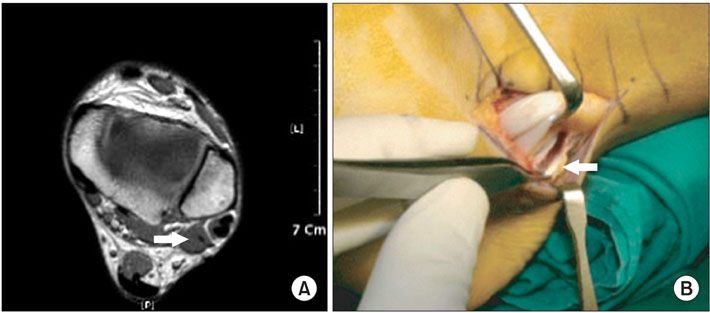
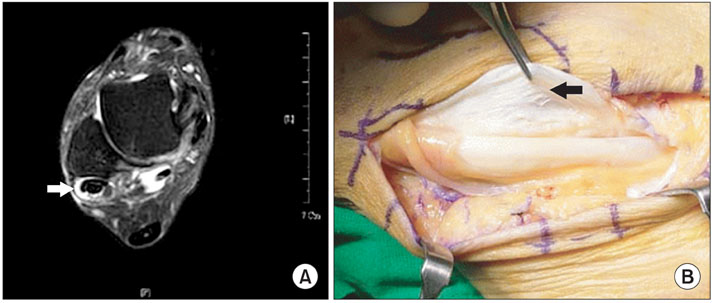
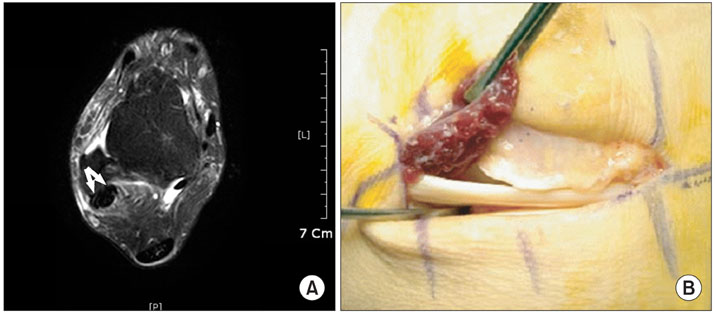
Of the 82 cases, 26 were true positives, 38 true negatives, 13 false positives and 5 false negatives. Of 39 cases of peroneal tendinopathy diagnosed from MRI, 14 had peroneal tendon partial tears, 15 tenosynovitis, 3 dislocations, 17 low-lying muscle bellies, and 6 peroneus quartus muscles. Of 31 cases of peroneal tendinopathy observed in surgery 11 had peroneal tendon partial tears, 4 tenosynovitis, 5 dislocations, 12 low-lying muscle belliess, and 1 peroneus quartus muscle. Sensitivity and specificity of peroneal tendinopathy were 83.9% and 74.5%, respectively. Positive predictive value was 66.7%. Negative predictive value was 88.4%. Accuracy rate was 78.0%.
CONCLUSIONS
MRI is a useful diagnostic tool for detecting peroneal tendinopathy in patients with chronic lateral ankle instability. However, MRI is vague in many cases. Therefore, a thorough delicate physical examination and careful observation is needed.
MeSH Terms
-
Adolescent
Adult
*Ankle Joint/surgery
Chronic Disease
Female
Humans
Joint Instability/*complications/surgery
*Magnetic Resonance Imaging
Male
Middle Aged
Observer Variation
Predictive Value of Tests
Sensitivity and Specificity
Tendinopathy/*diagnosis/etiology/surgery
Tendon Injuries/complications/diagnosis
Young Adult
Figure
Cited by 1 articles
-
Chronic Lateral Ankle Instability
Su-Young Bae
J Korean Foot Ankle Soc. 2020;24(1):1-8. doi: 10.14193/jkfas.2020.24.1.1.
Reference
-
1. Yao L, Tong DJ, Cracchiolo A, Seeger LL. MR findings in peroneal tendonopathy. J Comput Assist Tomogr. 1995. 19(3):460–464.
Article2. Sobel M, Geppert MJ, Olson EJ, Bohne WH, Arnoczky SP. The dynamics of peroneus brevis tendon splits: a proposed mechanism, technique of diagnosis, and classification of injury. Foot Ankle. 1992. 13(7):413–422.
Article3. Ferran NA, Maffulli N. Epidemiology of sprains of the lateral ankle ligament complex. Foot Ankle Clin. 2006. 11(3):659–662.
Article4. DIGiovanni BF, Fraga CJ, Cohen BE, Shereff MJ. Associated injuries found in chronic lateral ankle instability. Foot Ankle Int. 2000. 21(10):809–815.
Article5. Wang XT, Rosenberg ZS, Mechlin MB, Schweitzer ME. Normal variants and diseases of the peroneal tendons and superior peroneal retinaculum: MR imaging features. Radiographics. 2005. 25(3):587–602.
Article6. Hubbard TJ, Kramer LC, Denegar CR, Hertel J. Contributing factors to chronic ankle instability. Foot Ankle Int. 2007. 28(3):343–354.
Article7. Lee MS, Hofbauer MH. Evaluation and management of lateral ankle injuries. Clin Podiatr Med Surg. 1999. 16(4):659–678.8. Saxena A, Pham B. Longitudinal peroneal tendon tears. J Foot Ankle Surg. 1997. 36(3):173–179.
Article9. Tjin A Ton ER, Schweitzer ME, Karasick D. MR imaging of peroneal tendon disorders. AJR Am J Roentgenol. 1997. 168(1):135–140.
Article10. Lamm BM, Myers DT, Dombek M, Mendicino RW, Catanzariti AR, Saltrick K. Magnetic resonance imaging and surgical correlation of peroneus brevis tears. J Foot Ankle Surg. 2004. 43(1):30–36.
Article11. Kijowski R, De Smet A, Mukharjee R. Magnetic resonance imaging findings in patients with peroneal tendinopathy and peroneal tenosynovitis. Skeletal Radiol. 2007. 36(2):105–114.
Article12. Gray JM, Alpar EK. Peroneal tenosynovitis following ankle sprains. Injury. 2001. 32(6):487–489.
Article13. Cheung YY, Rosenberg ZS, Ramsinghani R, Beltran J, Jahss MH. Peroneus quartus muscle: MR imaging features. Radiology. 1997. 202(3):745–750.
Article14. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979. 86(2):420–428.
Article15. Dombek MF, Orsini R, Mendicino RW, Saltrick K. Peroneus brevis tendon tears. Clin Podiatr Med Surg. 2001. 18(3):409–427.16. Bencardino JT, Rosenberg ZS, Serrano LF. MR imaging features of diseases of the peroneal tendons. Magn Reson Imaging Clin N Am. 2001. 9(3):493–505.
Article17. Slater HK. Acute peroneal tendon tears. Foot Ankle Clin. 2007. 12(4):659–674.
Article18. Heckman DS, Reddy S, Pedowitz D, Wapner KL, Parekh SG. Operative treatment for peroneal tendon disorders. J Bone Joint Surg Am. 2008. 90(2):404–418.
Article19. Karlsson J, Wiger P. Longitudinal split of the peroneus brevis tendon and lateral ankle instability: treatment of concomitant lesions. J Athl Train. 2002. 37(4):463–466.20. Major NM, Helms CA, Fritz RC, Speer KP. The MR imaging appearance of longitudinal split tears of the peroneus brevis tendon. Foot Ankle Int. 2000. 21(6):514–519.
Article21. Alanen J, Orava S, Heinonen OJ, Ikonen J, Kvist M. Peroneal tendon injuries: report of thirty-eight operated cases. Ann Chir Gynaecol. 2001. 90(1):43–46.22. Sobel M, Bohne WH, Markisz JA. Cadaver correlation of peroneal tendon changes with magnetic resonance imaging. Foot Ankle. 1991. 11(6):384–388.
Article23. Sobel M, DiCarlo EF, Bohne WH, Collins L. Longitudinal splitting of the peroneus brevis tendon: an anatomic and histologic study of cadaveric material. Foot Ankle. 1991. 12(3):165–170.
Article24. Bonnin M, Tavernier T, Bouysset M. Split lesions of the peroneus brevis tendon in chronic ankle laxity. Am J Sports Med. 1997. 25(5):699–703.
Article25. Frey C, Bell J, Teresi L, Kerr R, Feder K. A comparison of MRI and clinical examination of acute lateral ankle sprains. Foot Ankle Int. 1996. 17(9):533–537.
Article26. Cardone BW, Erickson SJ, Den Hartog BD, Carrera GF. MRI of injury to the lateral collateral ligamentous complex of the ankle. J Comput Assist Tomogr. 1993. 17(1):102–107.
Article27. Donley BG, Leyes M. Peroneus quartus muscle: a rare cause of chronic lateral ankle pain. Am J Sports Med. 2001. 29(3):373–375.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Peroneal Tendinopathy in Chronic Lateral Ankle Instability
- Diagnosis and Comorbidity of Chronic Ankle Instability
- Chronic Lateral Ankle Instability
- Ligament Repair in Chronic Lateral Ankle Instability: Efficacy and Technique of Broström Procedures
- Diagnosis of Lateral Ankle Ligament Injury in the Evaluation of Chronic Lateral Ankle Instability