J Korean Med Sci.
2012 Aug;27(8):957-960. 10.3346/jkms.2012.27.8.957.
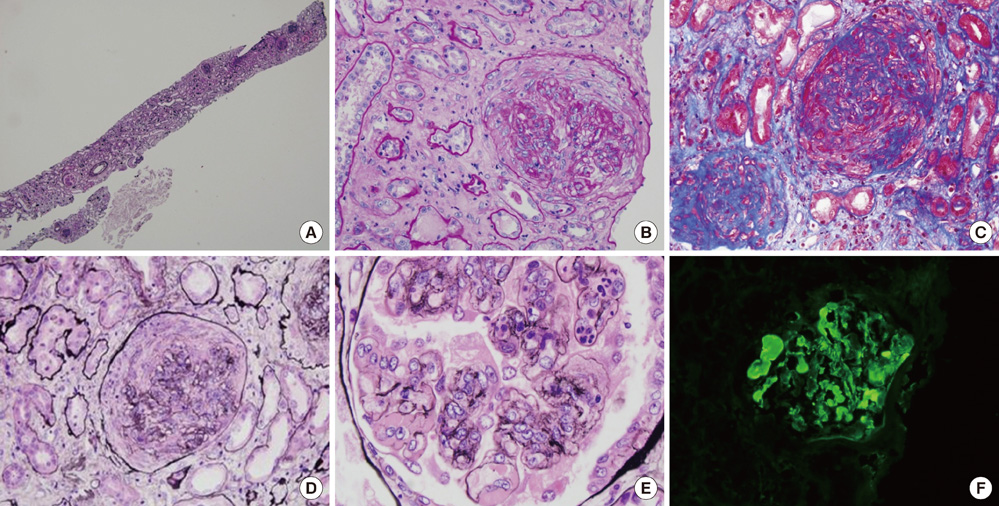
A Case of Elderly-Onset Crescentic Henoch-Schonlein Purpura Nephritis with Hypocomplementemia and Positive MPO-ANCA
- Affiliations
-
- 1Division of Nephrology, Department of Internal Medicine, Sungkyunkwan University School of Medicine, Seoul, Korea. kyubeck.lee@samsung.com
- 2Department of Pathology, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Pathology, Hanyang University College of Medicine, Seoul, Korea.
- KMID: 1714211
- DOI: http://doi.org/10.3346/jkms.2012.27.8.957
Abstract
- Henoch-Schonlein purpura (HSP) is common in childhood and often self-limiting. There have been limited studies on elderly-onset HSP nephritis (HSPN). A 76-yr-old man was transferred to our hospital with a 1-month history of oliguria, abdominal pain, edema and palpable purpura in the legs. Three months ago, he was admitted to another hospital with jaundice, and consequently diagnosed with early common bile duct cancer. The patient underwent a Whipple's operation. Antibiotics were administrated because of leakage in the suture from the surgery. However, he showed progressive renal failure with edema and purpura in the legs. Laboratory investigations showed serum creatinine 6.4 mg/dL, 24-hr urine protein 8,141 mg/day, myeloperoxidase anti-neutrophil cytoplasmic antibodies (MPO-ANCA) 1:40 and C3 below 64.89 mg/dL. Renal biopsy showed crescentic glomerulonephritis, as well as mesangial and extracapillary Ig A deposition. We started steroid therapy and hemodialysis, but he progressed to end-stage renal failure and he has been under maintenance hemodialysis. We describe elderly onset HSPN with MPO-ANCA can be crescentic glomerulonephritis rapidly progressed to end stage renal failure.
MeSH Terms
-
Aged
Antibodies, Antineutrophil Cytoplasmic/*analysis
Common Bile Duct Neoplasms/complications/surgery
Complement C3/analysis
Creatinine/blood
Edema/drug therapy
Enzyme-Linked Immunosorbent Assay
Glomerulonephritis/pathology
Humans
Male
Purpura, Schoenlein-Henoch/*diagnosis/drug therapy
Renal Dialysis
Renal Insufficiency/etiology/pathology
Steroids/therapeutic use
Antibodies, Antineutrophil Cytoplasmic
Complement C3
Steroids
Creatinine
Figure
Reference
-
1. Blanco R, Martínez-Taboada VM, Rodríguez-Valverde V, García-Fuentes M, González-Gay MA. Henoch-Schönlein purpura in adulthood and childhood: two different expressions of the same syndrome. Arthritis Rheum. 1997. 40:859–864.2. Pillebout E, Thervet E, Hill G, Alberti C, Vanhille P, Nochy D. Henoch-Schönlein purpura in adults: outcome and prognostic factors. J Am Soc Nephrol. 2002. 13:1271–1278.3. Diehl MP, Harrington T, Olenginski T. Elderly onset Henoch-Schönlein purpura: a case series and review of the literature. J Am Geriatr Soc. 2008. 56:2157–2159.4. Davin JC, Berge IJ, Weening JJ. What is the difference between IgA nephropathy and Henoch-Schönlein purpura nephritis. Kidney Int. 2001. 59:823–834.5. Krause I, Garty BZ, Davidovits M, Cleper R, Tamary H, Rosenmann E, Eisenstein B. Low serum C3, leukopenia, and thrombocytopenia: unusual features of Henoch-Schönlein purpura. Eur J Pediatr. 1999. 158:906–909.6. Kim NH, Ham YR, Yoon JH, Jung JY, Kim ES, Chung S, Choi DE, Na KR, Lee KW, Shin YT. Henoch-Schönlein nephritis in adults: renal outcomes and prognostic factors. Korean J Nephrol. 2009. 28:570–578.7. Shrestha S, Sumingan N, Tan J, Alhous H, McWilliam L, Ballardie F. Henoch-Schönlein purpura with nephritis in adults: adverse prognostic indicators in a UK population. QJM. 2006. 99:253–265.8. Rai A, Nast C, Adler S. Henoch-Schönlein purpura nephritis. J Am Soc Nephrol. 1999. 10:2637–2644.9. Yang YH, Chuang YH, Wang LC, Huang HY, Gershwin ME, Chiang BL. The immunobiology of Henoch-Schönlein purpura. Autoimmun Rev. 2008. 7:179–184.10. Lofters WS, Pineo GF, Luke KH, Yaworsky RG. Henoch-Schönlein purpura occurring in three members of a family. Can Med Assoc J. 1973. 109:46–48.11. Bollée G, Noël LH, Suarez F, Royal V, Gilardin L, de Serre NP, El-Ghoul B, Lesavre P, Alyanakian MA, Fakhouri F. Pauci-immune crescentic glomerulonephritis associated with ANCA of IgA class. Am J Kidney Dis. 2009. 53:1063–1067.12. Nagasaka T, Miyamoto J, Ishibashi M, Chen KR. MPO-ANCA- and IgA-positive systemic vasculitis: a possibly overlapping syndrome of microscopic polyangiitis and Henoch-Schöenlein purpura. J Cutan Pathol. 2009. 36:871–877.13. Bartůnková J, Tesar V, Sedivá A. Diagnostic and pathogenetic role of antineutrophil cytoplasmic autoantibodies. Clin Immunol. 2003. 106:73–82.14. Davin JC. Henoch-Schönlein purpura nephritis: pathophysiology, treatment, and future strategy. Clin J Am Soc Nephrol. 2011. 6:679–689.15. Hauer HA, Bajema IM, van Houwelingen HC, Ferrario F, Noël LH, Waldherr R, Jayne DR, Rasmussen N, Bruijn JA, Hagen EC. Renal histology in ANCA-associated vasculitis: differences between diagnostic and serologic subgroups. Kidney Int. 2002. 61:80–89.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Henoch-Schonlein Purpura after Abdominal Blunt Trauma
- A Case of Microscopic Polyangiitis Initially Suspected with Henoch-Schonlein Purpura Nephritis
- Changes of immune indices in children with recurrent gross hematuria (IgA nephropathy and non-IgA nephropathy) and Henoch-Schonlein purpura nephritis
- Clinicopathological Features and Outcomes of Childhood Henoch-Schonlein Purpura Nephritis
- A Clinicopathological Study on the Biopsy-proven Henoch-Schonlein Purpura Nephritis in Children