J Korean Med Sci.
2010 Aug;25(8):1253-1255. 10.3346/jkms.2010.25.8.1253.
Endobronchial Stent Insertion to Manage Hemoptysis caused by Lung Cancer
- Affiliations
-
- 1Department of Radiology, Dankook University College of Medicine, Cheonan, Korea. hae0820@naver.com
- 2Division of Pulmonology and Allergy, Department of Internal Medicine, Dankook University College of Medicine, Cheonan, Korea.
- KMID: 1714056
- DOI: http://doi.org/10.3346/jkms.2010.25.8.1253
Abstract
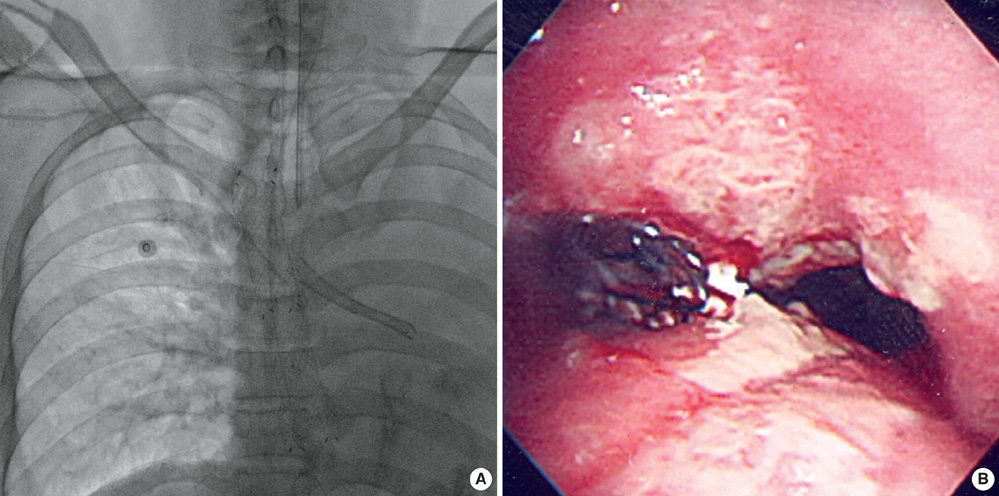
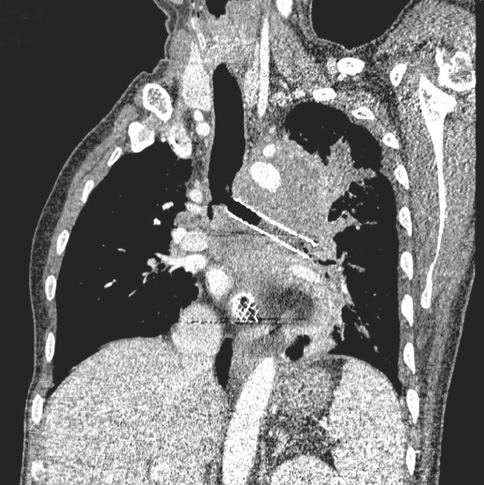
- Hemoptysis in patients with lung cancer is not uncommon and sometimes have dangerous consequences. Hemoptysis has been managed with various treatment options other than surgery and medicine, such as endobronchial tamponade, transcatheter arterial embolization and radiation therapy. However, these methods can sometimes be used only temporarily or are not suitable for a patient's condition. We present a case in which uncontrollable hemoptysis caused by central lung cancer was successfully treated by inserting a covered self-expanding bronchial stent. The patient could be extubated and was able to undergo further palliative therapy. No recurrent episodes of hemoptysis occurred for the following three months. As our case, airway stenting is a considerable option for the tamponade of a bleeding lesion that cannot be successfully managed with other treatment methods and could be used to preserve airway patency in a select group of patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Chute CG, Greenberg ER, Baron J, Korson R, Baker J, Yates J. Presenting conditions of 1539 population-based lung cancer patients by cell type and stage in New Hampshire and Vermont. Cancer. 1985. 56:2107–2111.
Article2. Miller RR, McGregor DH. Hemorrhage from carcinoma of the lung. Cancer. 1980. 46:200–205.
Article3. Dweik RA, Stoller JK. Role of bronchoscopy in massive hemoptysis. Clin Chest Med. 1999. 20:89–105.
Article4. Johnson JL. Manifestations of hemoptysis. How to manage minor, moderate, and massive bleeding. Postgrad Med. 2002. 112:101–106. 108–109. 1135. Langendijk JA, ten Velde GP, Aaronson NK, de Jong JM, Muller MJ, Wouters EF. Quality of life after palliative radiotherapy in non-small cell lung cancer: a prospective study. Int J Radiat Oncol Biol Phys. 2000. 47:149–155.
Article6. Mal H, Rullon I, Mellot F, Brugiere O, Sleiman C, Menu Y, Fournier M. Immediate and long-term results of bronchial artery embolization for life-threatening hemoptysis. Chest. 1999. 115:996–1001.
Article7. Osaki S, Nakanishi Y, Wataya H, Takayama K, Inoue K, Takaki Y, Murayama S, Hara N. Prognosis of bronchial artery embolization in the management of hemoptysis. Respiration. 2000. 67:412–416.
Article8. Kvale PA, Simoff M, Prakash UB. Lung cancer. Palliative care. Chest. 2003. 123:1 Suppl. 284S–311S.9. Brandes JC, Schmidt E, Yung R. Occlusive endobronchial stent placement as a novel management approach to massive hemoptysis from lung cancer. J Thorac Oncol. 2008. 3:1071–1072.
Article10. Nam DH, Shin JH, Song HY, Jung GS, Han YM. Malignant esophageal-tracheobronchial strictures: parallel placement of covered retrievable expandable nitinol stents. Acta Radiol. 2006. 47:3–9.
Article11. Onishi H, Kuriyama K, Komiyama T, Tanaka S, Marino K, Tsukamoto T, Araki T. A case of aorto-bronchial fistula after insertion of left main bronchial self-expanding metallic stent in a patient with recurrent esophageal cancer. Cardiovasc Intervent Radiol. 2004. 27:288–290.
Article12. Song HY, Shim TS, Kang SG, Jung GS, Lee DY, Kim TH, Park S, Ahn YM, Kim WS. Tracheobronchial strictures: treatment with a polyurethane-covered retrievable expandable nitinol stent--initial experience. Radiology. 1999. 213:905–912.
Article13. Kim JH, Shin JH, Song HY, Shim TS, Yoon CJ, Ko GY. Benign tracheobronchial strictures: long-term results and factors affecting airway patency after temporary stent placement. AJR Am J Roentgenol. 2007. 188:1033–1038.
Article14. Miyazawa T, Yamakido M, Ikeda S, Furukawa K, Takiguchi Y, Tada H, Shirakusa T. Implantation of ultraflex nitinol stents in malignant tracheobronchial stenoses. Chest. 2000. 118:959–965.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Covered Bronchial Stent Insertion to Manage Airway Obstruction with Hemoptysis Caused by Lung Cancer
- A Case of Complication of Expandible Metallic Stent with Endobronchial Stenosis
- Photodynamic Therapy for Endobronchial Obstruction due to Recurrent Lung Cancer : 2 Cases Report
- Updates in diagnostic bronchoscopy for lung cancer
- A case of endobronchial aspergilloma with massive hemoptysis