J Korean Med Sci.
2008 Apr;23(2):251-255. 10.3346/jkms.2008.23.2.251.
The Significance of Gastric Juice Analysis for a Positive Challenge by a Standard Oral Challenge Test in Typical Cow's Milk Protein-Induced Enterocolitis
- Affiliations
-
- 1Department of Pediatrics, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea. pedgi@kmu.ac.kr
- 2Institute for Medical Science, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea.
- 3Department of Preventive Medicine, Kyungpook National University School of Medicine, Daegu, Korea.
- 4Department of Pediatrics, Hyosung Medical Center, Daegu, Korea.
- KMID: 1713457
- DOI: http://doi.org/10.3346/jkms.2008.23.2.251
Abstract
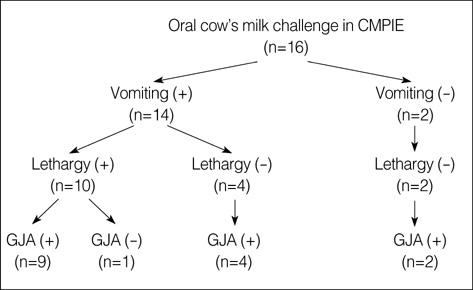
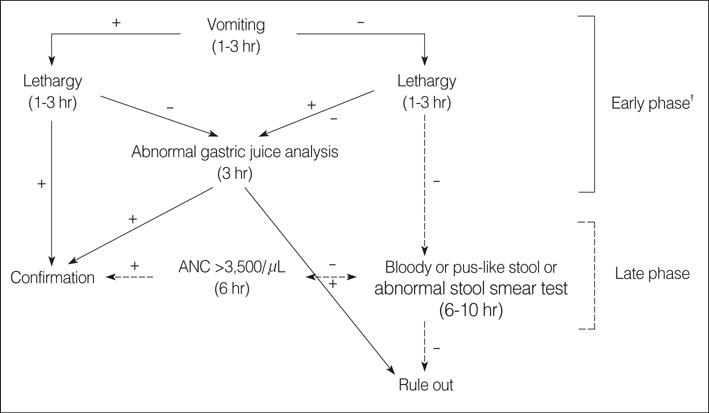
- This study was performed to investigate the significance of gastric juice analysis (GJA) as a diagnostic criterion of a positive challenge in a standard oral cow's milk challenge (OCC) to confirm typical cow's milk protein-induced enterocolitis (CMPIE). Data from 16 CMPIE patients (aged 14 to 44 days) were analyzed. A standard OCC was openly executed using 0.15 g/kg of protein. Three symptoms (vomiting, lethargy, and bloody or pus-like stool), and four laboratory findings (GJA [3 hr], changes in peripheral blood absolute neutrophil count [ANC] [6 hr], C-reactive protein [6 hr], and stool smear test for occult blood or leukocytes) were observed after OCC. Before OCC, baseline studies were conducted; a stool smear test, blood sampling, and GJA. Positive OCC results were; vomiting (87.5%) (observed 1-3 hr after OCC), lethargy (62.5%) (1-3 hr), bloody or pus-like stool (43.8%) (6-10 hr), abnormal GJA (93.8%), an ANC rise >3,500 cells/microliter (93.8%), and an abnormal stool smear test (75.0%). A single GJA test after a standard OCC is a sensitive diagnostic criterion of a positive challenge, and may provide an early confirmatory diagnosis of CMPIE. An investigation of positive OCC outcomes helps to find out a diagnostic algorithm of criteria of a positive challenge in CMPIE.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Clinical Perspectives of Food Allergy in Infants and Young Children
Jin-Bok Hwang
Korean J Pediatr Gastroenterol Nutr. 2011;14(2):113-121. doi: 10.5223/kjpgn.2011.14.2.113.The Characteristics and Diagnostic Methods of Food Protein Induced Proctocolitis
Ae Suk Kim, Jin-Bok Hwang
Korean J Pediatr Gastroenterol Nutr. 2011;14(Suppl 1):S47-S54. doi: 10.5223/kjpgn.2011.14.Suppl1.S47.Is This Symptom Even a Food Allergy?: Clinical Types of Food Protein-induced Enterocolitis Syndrome
Jin-Bok Hwang
Pediatr Gastroenterol Hepatol Nutr. 2014;17(2):74-79. doi: 10.5223/pghn.2014.17.2.74.
Reference
-
1. Sicherer SH, Eigenmann PA, Sampson HA. Clinical features of food protein-induced enterocolitis syndrome. J Pediatr. 1998. 133:214–219.
Article2. Powell GK. Milk- and soy-induced enterocolitis of infancy. Clinical features and standardization of challenge. J Pediatr. 1978. 93:553–560.3. Powell GK. Food protein-induced enterocolitis of infancy: Differential diagnosis and management. Compr Ther. 1986. 12:28–37.4. Burks AW, Casteel HB, Fiedorek SC, Williams LW, Pumphrey CL. Prospective oral food challenge study of two soybean protein isolates in patients with possible milk or soy protein enterocolitis. Pediatr Allergy Immunol. 1994. 5:40–45.
Article5. Sicherer SH. Food protein-induced enterocolitis syndrome: case presentations and management lessons. J Allergy Clin Immunol. 2005. 115:149–156.
Article6. Fogg MI, Brown-Whitehorn TA, Pawlowski NA, Spergel JM. Atopy patch test for the diagnosis of food protein-induced enterocolitis syndrome. Pediatr Allergy Immunol. 2006. 17:351–355.
Article7. Sicherer SH. Food allergy: when and how to perform oral food challenges. Pediatr Allergy Immunol. 1999. 10:226–234.
Article8. Sicherer SH. Clinical aspects of gastrointestinal food allergy in childhood. Pediatrics. 2003. 111:1609–1616.9. Chung HL, Hwang JB, Park JJ, Kim SG. Expression of transforming growth factor beta1, transforming growth factor type I and II receptors, and TNF-alpha in the mucosa of the small intestine in infants with food protein-induced enterocolitis syndrome. J Allergy Clin Immunol. 2002. 109:150–154.10. Murray KF, Christie DL. Dietary protein intolerance in infants with transient methemoglobinemia and diarrhea. J Pediatr. 1993. 122:90–92.
Article11. Hwang JB, Lee SH, Kang YN, Kim SP, Suh SI, Kam S. Indexes of suspicion of typical cow's milk protein-induced enterocolitis. J Korean Med Sci. 2007. 22:993–997.
Article12. McDonald PJ, Goldblum RM, Van Sickle GJ, Powell GK. Food protein-induced enterocolitis: altered antibody response to ingested antigen. Pediatr Res. 1984. 18:751–755.
Article13. Scarborough DR, Isaacson LG. Hypothetical anatomical model to describe the aberrant gag reflex observed in a clinical population of orally deprived children. Clin Anat. 2006. 19:640–644.
Article14. Nowak-Wegrzyn A, Sampson HA, Wood RA, Sicherer SH. Food protein-induced enterocolitis syndrome caused by solid food proteins. Pediatrics. 2003. 111:829–835.
Article