J Korean Med Sci.
2007 Apr;22(2):330-335. 10.3346/jkms.2007.22.2.330.
One-year Outcome Evaluation after Interspinous Implantation for Degenerative Spinal Stenosis with Segmental Instability
- Affiliations
-
- 1Department of Neurosurgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, 50 Ilwon-dong, Gangnam-gu, Seoul, Korea. kimes@smc.samsung.co.kr
- KMID: 1713196
- DOI: http://doi.org/10.3346/jkms.2007.22.2.330
Abstract
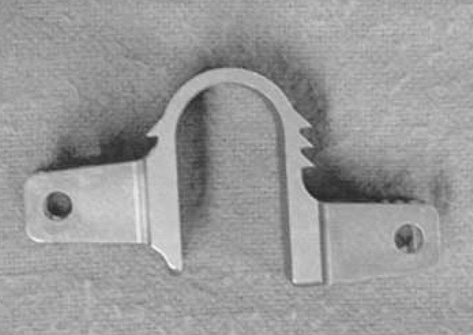
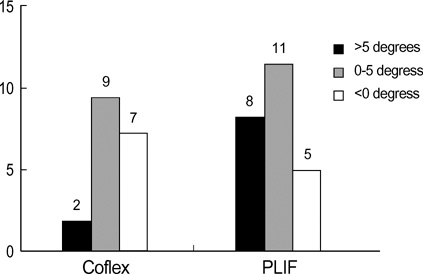
- The authors hypothesized that the placement of the interspinous implant would show a similar clinical outcome to the posterior lumbar interbody fusion (PLIF) in patients having spinal stenosis with mild segmental instability and that this method would be superior to PLIF without significantly affecting degeneration at the adjacent segments. Forty two adult patients having degenerative spinal stenosis with mild segmental instabilit who underwent implantation of Coflex(TM) (Spine motion, Germany) or PLIF at L4-5 between January 2000 and December 2003 were consecutively selected and studied for one-year clinical outcome. At 12 months after surgery, both groups showed a significant improvement in the visual analogue scale score and Oswestry disability index score for both lower extremity pain and low back pain. However, the range of motion at the upper adjacent segments (L3-4) increased significantly after surgery in the PLIF group, which was not manifested in the Coflex(TM) group during the follow-up. The authors assumed that interspinous implantation can be an alternative treatment for the spinal stenosis with segmental instability in selected conditions posing less stress on the superior adjacent level than PLIF.
Keyword
MeSH Terms
-
Treatment Outcome
Spinal Stenosis/complications/*surgery
Spinal Fusion/*instrumentation/methods
Prosthesis Design
Pain Measurement
Outcome Assessment (Health Care)
Middle Aged
Male
Lumbar Vertebrae/*surgery
Longitudinal Studies
Joint Instability/complications/*prevention & control
Intermittent Claudication/diagnosis/etiology/*prevention & control
Humans
Female
Equipment Failure Analysis
Back Pain/diagnosis/etiology/*prevention & control
Aged
Adult
Figure
Reference
-
1. Verbiest H. A radicular syndrome from developmental narrowing of the lumbae vertebral canal. J Bone Joint Surg. 1954. 36-B:230–237.2. Etebar S, Cahill DW. Risk factors for adjacent-segment failure following lumbar fixation with rigid instrumentation for degenerative instability. J Neurosurg. 1999. 90:163–169.
Article3. Kanayama M, Hashimoto T, Shigenobu K, Harada M, Oha F, Ohkoshi Y, Tada H, Yamamoto K, Yamane S. Adjacent-segment morbidity after Graf ligamentoplasty compared with posterolateral lumbar fusion. J Neurosurg. 2001. 95:Suppl 1. 5–10.
Article4. Lee CK. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine. 1988. 13:375–377.
Article5. Swanson KE, Lindsey DP, Hsu KY, Zucherman JF, Yerby SA. The effects of an interspinous implant on intervertebral disc pressures. Spine. 2003. 28:26–32.
Article6. Zucherman JF, Hsu KY, Hartjen CA, Mehalic TF, Implicito DA, Martin MJ, Johnson DR 2nd, Skidmore GA, Vessa PP, Dwyer JW, Puccio S, Cauthen JC, Ozuna RM. A prospective randomized multicenter study for the treatment of lumbar spinal stenosis with the X STOP interspinous implant: 1-year results. Eur Spine J. 2004. 13:22–31.
Article7. Kaech DL, Jinkins JR. The interspinous 'U': a new restabilization device for the lumbar spine Spinal Restabilization Procedures. 2002. Elsevier Science B.V.;355–362.8. Amundsen T, Weber H, Lilleas F, Nordal HJ, Abdelnoor M, Magnaes B. Lumbar spinal stenosis. Clinical and radiologic features. Spine. 1995. 20:1178–1186.9. Bridwell KH, Sedgewick TA, O'Brien MF, Lenke LG, Baldus C. The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Disord. 1993. 6:461–472.
Article10. West JL 3rd, Bradford DS, Ogilvie JW. Results of spinal arthrodesis with pedicle screw-plate fixation. J Bone Joint Surg Am. 1991. 73:1179–1184.
Article11. Cunningham BW, Kotani Y, McNulty PS, Cappuccino A, McAfee PC. The effect of spinal destabilization and instrumentation on lumbar intradiscal pressure: an in vitro biomechanical analysis. Spine. 1997. 22:2655–2663.12. Schlegel JD, Smith JA, Schleusener RL. Lumbar motion segment pathology adjacent to thoracolumbar, lumbar, and lumbosacral fusions. Spine. 1996. 21:970–981.
Article13. Penta M, Sandhu A, Fraser RD. Magnetic resonance imaging assessment of disc degeneration 10 years after anterior lumbar interbody fusion. Spine. 1995. 20:743–747.
Article14. Korovessis P, Papazisis Z, Koureas G, Lambiris E. Rigid, semirigid versus dynamic instrumentation for degenerative lumbar spinal stenosis: a correlative radiological and clinical analysis of short-term results. Spine. 2004. 29:735–742.15. Lee J, Hida K, Seki T, Iwasaki Y, Minoru A. An interspinous process distractor (X STOP) for lumbar spinal stenosis in elderly patients: preliminary experiences in 10 consecutive cases. J Spinal Disord Tech. 2004. 17:72–77. discussion 78.16. Lindsey DP, Swanson KE, Fuchs P, Hsu KY, Zacherman JF, Yerby SA. The effects of an interspinous implant on the kinematics of the instrumented and adjacent levels in the lumbar spine. Spine. 2003. 28:2192–2197.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preliminary Report on Usefulness of Adjacent Interspinous Stabilization using Interspinous Spacer Combined with Posterior Lumbosacral Spinal Fusion in Degenerative Lumbar Disease
- Late Complications of the Single Level 'Interspinous U' in Lumbar Spinal Stenosis with Mild Segmental Instability
- Treatment of Degenerative Lumbar Stenosis with Minimal Decompression
- Long-term Follow-up (Minimum 5 Years) Study of Single-level Posterior Dynamic Stabilization in Lumbar Degenerative Disease; 'Interspinous U' & 'DIAM'
- Efficacy of Dynamic Radiographs in Routine Evaluations for Degenerative Cervical Spine Disease