J Gynecol Oncol.
2014 Apr;25(2):97-104. 10.3802/jgo.2014.25.2.97.
Cost-utility analysis of treatments for stage IB cervical cancer
- Affiliations
-
- 1Radiation Oncology Unit, Department of Radiology, Faculty of Medicine Vajira Hospital, Navamindradhiraj University, Bangkok, Thailand. Kankatanyoo@edu.vajira.ac.th
- 2Health Intervention and Technology Assessment Program & Bureau of AIDS, TB and STIs, Department of Disease Control, Ministry of Public Health, Nonthaburi, Thailand.
- 3Gynecologic Oncology Unit, Department of Obstetrics and Gynecology, Faculty of Medicine Vajira Hospital, Navamindradhiraj University, Bangkok, Thailand.
- 4Clinical Epidemiology Unit, Faculty of Medicine Vajira Hospital, Navamindradhiraj University, Bangkok, Thailand.
- KMID: 1708331
- DOI: http://doi.org/10.3802/jgo.2014.25.2.97
Abstract
OBJECTIVE
To analyze the cost-utility of two common clinical practices for stage IB cervical cancer patients from provider and societal viewpoints.
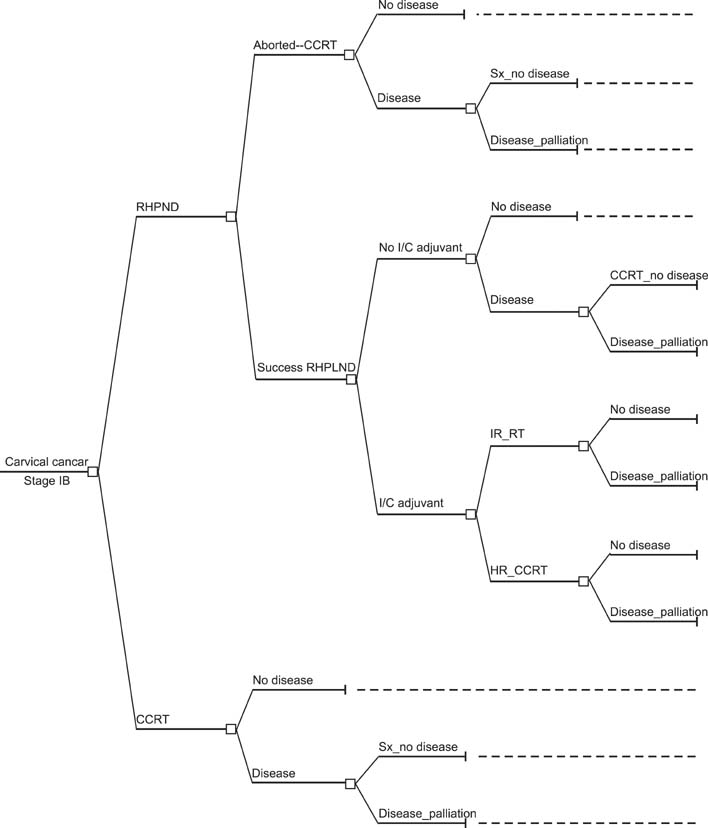
METHODS
A decision tree model was conducted to examine value for expenditure between the following: (1) radical hysterectomy with pelvic lymph node dissection (RHPLND) with or without postoperative adjuvant therapy according to the risk of recurrence and (2) concurrent chemoradiotherapy (CCRT). The relevant studies were identified to extract the probability data, and meta-analysis was performed. Direct medical costs were estimated from hospital database and medical records review. Direct non-medical costs and utility parameters were obtained through interviews with patients to estimate quality-adjusted life years (QALYs) outcome. The time horizon was according to the life expectancy of Thai women.
RESULTS
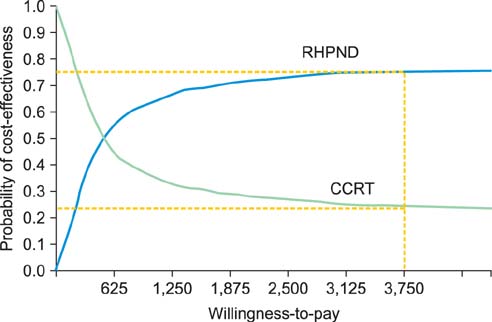
From provider viewpoint, RHPLND and CCRT resulted in approximate costs of US $5,281 and US $5,218, respectively. The corresponding costs from societal viewpoint were US $6,533 and US $6,335, respectively. QALYs were 16.40 years for RHPLND and 15.94 years for CCRT. The estimated incremental cost effectiveness ratio of RHPLND in comparison to CCRT from provider and societal viewpoints were US $100/QALY and US $430/QALY, respectively. RHPLND had more cost-effectiveness than CCRT if patients did not need adjuvant therapy. The most effective parameter in model was a direct medical cost of CCRT. At the current ceiling ratio in Thailand, RHPLND provides better value for money than CCRT, with a probability of 75%.
CONCLUSION
RHPLND is an efficient treatment for stage IB cervical cancer. This advantage is only for patients who require no adjuvant treatment.
Keyword
MeSH Terms
Figure
Reference
-
1. Sriplung H, Wiangnon S, Sontipong S, Sumitsawan Y, Martin N. Cancer incidence trends in Thailand, 1989-2000. Asian Pac J Cancer Prev. 2006; 7:239–244.2. Hopkins MP, Morley GW. Radical hysterectomy versus radiation therapy for stage IB squamous cell cancer of the cervix. Cancer. 1991; 68:272–277.3. Landoni F, Maneo A, Colombo A, Placa F, Milani R, Perego P, et al. Randomised study of radical surgery versus radiotherapy for stage Ib-IIa cervical cancer. Lancet. 1997; 350:535–540.4. Keys HM, Bundy BN, Stehman FB, Muderspach LI, Chafe WE, Suggs CL 3rd, et al. Cisplatin, radiation, and adjuvant hysterectomy compared with radiation and adjuvant hysterectomy for bulky stage IB cervical carcinoma. N Engl J Med. 1999; 340:1154–1161.5. Monk BJ, Wang J, Im S, Stock RJ, Peters WA 3rd, Liu PY, et al. Rethinking the use of radiation and chemotherapy after radical hysterectomy: a clinical-pathologic analysis of a Gynecologic Oncology Group/Southwest Oncology Group/Radiation Therapy Oncology Group trial. Gynecol Oncol. 2005; 96:721–728.6. Sedlis A, Bundy BN, Rotman MZ, Lentz SS, Muderspach LI, Zaino RJ. A randomized trial of pelvic radiation therapy versus no further therapy in selected patients with stage IB carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy: A Gynecologic Oncology Group Study. Gynecol Oncol. 1999; 73:177–183.7. Peters WA 3rd, Liu PY, Barrett RJ 2nd, Stock RJ, Monk BJ, Berek JS, et al. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncol. 2000; 18:1606–1613.8. Stehman FB, Ali S, Keys HM, Muderspach LI, Chafe WE, Gallup DG, et al. Radiation therapy with or without weekly cisplatin for bulky stage 1B cervical carcinoma: follow-up of a Gynecologic Oncology Group trial. Am J Obstet Gynecol. 2007; 197:503.e1–503.e6.9. Chang SJ, Kim WY, Yoo SC, Yoon JH, Chun M, Chang KH, et al. A validation study of new risk grouping criteria for postoperative treatment in stage IB cervical cancers without high-risk factors: rethinking the Gynecologic Oncology Group criteria. Eur J Obstet Gynecol Reprod Biol. 2009; 147:91–96.10. Is pelvic radiation beneficial in the postoperative management of stage Ib squamous cell carcinoma of the cervix with pelvic node metastasis treated by radical hysterectomy and pelvic lymphadenectomy? A report from the Presidential Panel at the 1979 Annual Meeting of the Society of Gynecologic Oncologists. Gynecol Oncol. 1980; 10:105–110.11. Lyman GH, Levine M. Comparative effectiveness research in oncology: an overview. J Clin Oncol. 2012; 30:4181–4184.12. Rocconi RP, Estes JM, Leath CA 3rd, Kilgore LC, Huh WK, Straughn JM Jr. Management strategies for stage IB2 cervical cancer: a cost-effectiveness analysis. Gynecol Oncol. 2005; 97:387–394.13. Jewell EL, Kulasingam S, Myers ER, Alvarez Secord A, Havrilesky LJ. Primary surgery versus chemoradiation in the treatment of IB2 cervical carcinoma: a cost effectiveness analysis. Gynecol Oncol. 2007; 107:532–540.14. Phippen NT, Leath CA 3rd, Chino JP, Jewell EL, Havrilesky LJ, Barnett JC. Cost effectiveness of concurrent gemcitabine and cisplatin with radiation followed by adjuvant gemcitabine and cisplatin in patients with stages IIB to IVA carcinoma of the cervix. Gynecol Oncol. 2012; 127:267–272.15. Look KY, Rocereto TF. Relapse patterns in FIGO stage IB carcinoma of the cervix. Gynecol Oncol. 1990; 38:114–120.16. Thailand life expectancy at birth [Internet]. IndexMundi;c2013. cited 2012 Sep 30. Available from: http://www.indexmundi.com/thailand/life_expectancy_at_birth.html.17. Sardi JE, Giaroli A, Sananes C, Ferreira M, Soderini A, Bermudez A, et al. Long-term follow-up of the first randomized trial using neoadjuvant chemotherapy in stage Ib squamous carcinoma of the cervix: the final results. Gynecol Oncol. 1997; 67:61–69.18. Whitney CW, Stehman FB. The abandoned radical hysterectomy: a Gynecologic Oncology Group Study. Gynecol Oncol. 2000; 79:350–356.19. Leath CA 3rd, Straughn JM Jr, Estes JM, Kirby TO, Bhoola SM, Barnes MN 3rd, et al. The impact of aborted radical hysterectomy in patients with cervical carcinoma. Gynecol Oncol. 2004; 95:204–207.20. Cai HB, Chen HZ, Yin HH. Randomized study of preoperative chemotherapy versus primary surgery for stage IB cervical cancer. J Obstet Gynaecol Res. 2006; 32:315–323.21. Van de Putte G, Lie AK, Vach W, Baekelandt M, Kristensen GB. Risk grouping in stage IB squamous cell cervical carcinoma. Gynecol Oncol. 2005; 99:106–112.22. Rutledge TL, Kamelle SA, Tillmanns TD, Gould NS, Wright JD, Cohn DE, et al. A comparison of stages IB1 and IB2 cervical cancers treated with radical hysterectomy. Is size the real difference? Gynecol Oncol. 2004; 95:70–76.23. Rotman M, Sedlis A, Piedmonte MR, Bundy B, Lentz SS, Muderspach LI, et al. A phase III randomized trial of postoperative pelvic irradiation in Stage IB cervical carcinoma with poor prognostic features: follow-up of a gynecologic oncology group study. Int J Radiat Oncol Biol Phys. 2006; 65:169–176.24. Chaikledkaew U, Teerawattananon Y, Suksomboon N. Health intervention and technology assessment program. Nonthaburi, Thailand: Graphico Systems Co.;2009.25. Brooks R. EuroQol: the current state of play. Health Policy. 1996; 37:53–72.26. EuroQol Group. EuroQol: a new facility for the measurement of health-related quality of life. Health Policy. 1990; 16:199–208.27. Tongsiri S, Cairns J. Estimating population-based values for EQ-5D health states in Thailand. Value Health. 2011; 14:1142–1145.28. Napolitano U, Imperato F, Mossa B, Framarino ML, Marziani R, Marzetti L. The role of neoadjuvant chemotherapy for squamous cell cervical cancer (Ib-IIIb): a long-term randomized trial. Eur J Gynaecol Oncol. 2003; 24:51–59.29. Eddy GL, Bundy BN, Creasman WT, Spirtos NM, Mannel RS, Hannigan E, et al. Treatment of ("bulky") stage IB cervical cancer with or without neoadjuvant vincristine and cisplatin prior to radical hysterectomy and pelvic/para-aortic lymphadenectomy: a phase III trial of the gynecologic oncology group. Gynecol Oncol. 2007; 106:362–369.30. Kim HS, Sardi JE, Katsumata N, Ryu HS, Nam JH, Chung HH, et al. Efficacy of neoadjuvant chemotherapy in patients with FIGO stage IB1 to IIA cervical cancer: an international collaborative meta-analysis. Eur J Surg Oncol. 2013; 39:115–124.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgery or chemoradiation for stage IB cervical cancer? How cost effectiveness impacts a complex decision
- Cost-effectiveness of tisotumab vedotin as a second- or third-line therapy for cervical cancer
- The twenty-first century role of Piver-Rutledge type III radical hysterectomy and FIGO stage IA, IB1, and IB2 cervical cancer in the era of robotic surgery: a personal perspective
- Ovarian Metastasis from Stage IB Cervical Adenocarcinoma: A Case Report
- Cost-benefit issues about human papillomavirus (HPV) testing