Clin Orthop Surg.
2013 Jun;5(2):129-133. 10.4055/cios.2013.5.2.129.
The Efficacy of Carotid Tubercle as an Anatomical Landmark for Identification of Cervical Spinal Level in the Anterior Cervical Surgery: Comparison with Preoperative C-arm Fluoroscopy
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul Metropolitan Government Seoul National University Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea. jiholee@brm.co.kr
- 2Institute of Medical and Biological Engineering, Seoul National University Medical Research Center, Seoul, Korea.
- KMID: 1705534
- DOI: http://doi.org/10.4055/cios.2013.5.2.129
Abstract
- BACKGROUND
In cervical anterior approach, transverse skin incision is preferred due to cosmetic reasons. Precise skin incision is required to reach the surgery segment while minimizing soft tissue injury. Skin incision site is frequently identified using C-arm fluoroscopy or the carotid tubercle. Accordingly, this study was conducted to investigate the efficacy of skin incision using the carotid tubercle as a marker.
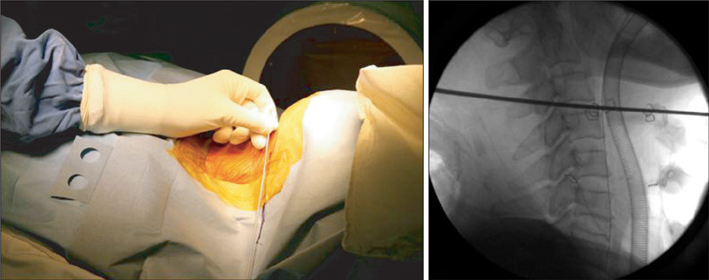
METHODS
This study was retrospectively conducted on 114 patients who underwent anterior cervical surgery by the same surgeon from April 2004 to June 2012. The rate of the appropriate insertion of K-wire, which was inserted into the disc after anterior approach, into the surgery segment was compared between 62 patients where skin incision site was identified using C-arm fluoroscopy before skin incision and 52 patients where skin incision site was identified using carotid tubercle palpitation before surgery.
RESULTS
The needle was shown to have been inserted into the planned site in 106 patients out of the total 114 patients. The appropriate insertion of the needle was shown in 59 patients of group I (95.2%) and in 47 patients of group II (90.4%). Although the success rate was higher in group I than group II, it was statistically insignificant. The success rate of one-segment surgery was shown to be 89.7% in group I and 82.6% in group II. Although the success rate was higher in group I than group II, it was statistically insignificant. The success rate of two-segment surgery was shown to be 100% in group I, and 96.4% in group II due to one case of the failure at C3-4 and C5-6. The success rate of three- and four-segment surgeries was shown to be 100% in both groups.
CONCLUSIONS
The identification of skin incision site via carotid tubercle palpation was useful for surgeries involving two or more segments. Furthermore, it could be useful for one-segment surgery if surgical site is identified using vertebral body or soft tissues such as longus collis rather than insertion into the disc.
MeSH Terms
Figure
Reference
-
1. Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958; 15(6):602–617.
Article2. Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958; 40(3):607–624.
Article3. Song KJ, Choi BW, Kim HY, Jeon TS, Chang H. Efficacy of postoperative radiograph for evaluating the prevertebral soft tissue swelling after anterior cervical discectomy and fusion. Clin Orthop Surg. 2012; 4(1):77–82.
Article4. Auerbach JD, Weidner Z, Pill SG, Mehta S, Chin KR. The mandibular angle as a landmark for identification of cervical spinal level. Spine (Phila Pa 1976). 2009; 34(10):1006–1011.
Article5. Zhang H, Yang S, Wang L, et al. Time course investigation of intervertebral disc degeneration produced by needle-stab injury of the rat caudal spine: laboratory investigation. J Neurosurg Spine. 2011; 15(4):404–413.
Article6. Michalek AJ, Buckley MR, Bonassar LJ, Cohen I, Iatridis JC. The effects of needle puncture injury on microscale shear strain in the intervertebral disc annulus fibrosus. Spine J. 2010; 10(12):1098–1105.
Article7. Zhang H, La Marca F, Hollister SJ, Goldstein SA, Lin CY. Developing consistently reproducible intervertebral disc degeneration at rat caudal spine by using needle puncture. J Neurosurg Spine. 2009; 10(6):522–530.
Article8. Lee K, Lee KM, Park MS, Lee B, Kwon DG, Chung CY. Measurements of surgeons exposure to ionizing radiation dose during intraoperative use of C-arm fluoroscopy. Spine (Phila Pa 1976). 2012; 37(14):1240–1244.
Article9. Civelek E, Kiris T, Hepgul K, Canbolat A, Ersoy G, Cansever T. Anterolateral approach to the cervical spine: major anatomical structures and landmarks: technical note. J Neurosurg Spine. 2007; 7(6):669–678.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effectiveness of Doppler Image of the Vertebral Artery as an Anatomical Landmark for Identification of Ultrasound-Guided Target Level in Cervical Spine
- An Anatomical Variant : Low-Lying Bifurcation of the Common Carotid Artery, and Its Surgical Implications in Anterior Cervical Discectomy
- Reliability and Accuracy of Palpable Anterior Neck Landmarks for the Identification of Cervical Spinal Levels
- Cervicothoracic Spinal Epidural Hematoma after Anterior Cervical Spinal Surgery
- Comparison between the coronal diameters of the cervical spinal canal and spinal cord measured using computed tomography and magnetic resonance imaging in Korean patients