Obstet Gynecol Sci.
2014 May;57(3):193-200. 10.5468/ogs.2014.57.3.193.
Prenatal diagnosis of atrial isomerism in the Korean population
- Affiliations
-
- 1Department of Obstetrics and Gynecology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. hswon@amc.seoul.kr
- 2Division of Neonatology, Department of Pediatrics, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 3Department of Pediatric Cardiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 4Division of Pediatric Cardiac Surgery, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- KMID: 1704425
- DOI: http://doi.org/10.5468/ogs.2014.57.3.193
Abstract
OBJECTIVE
To report our experiences in the prenatal diagnosis of atrial isomerism and postnatal outcomes.
METHODS
A total of 80 fetuses prenatally diagnosed with atrial isomerism were retrospectively analyzed between 1999 and 2011 at a single institution.
RESULTS
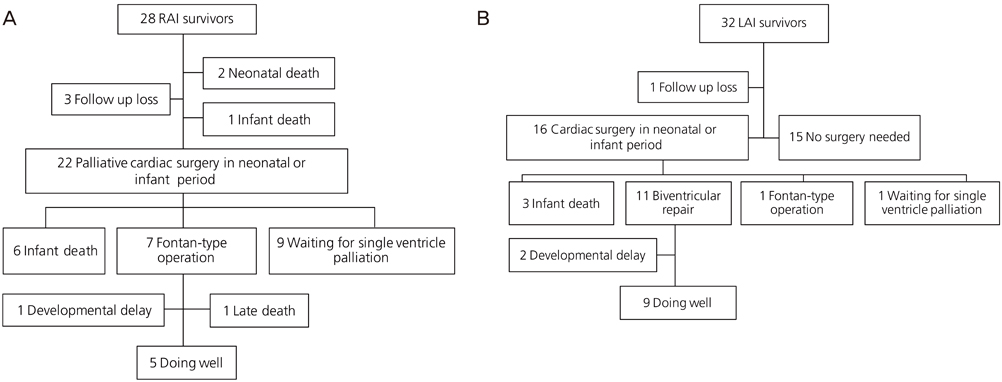
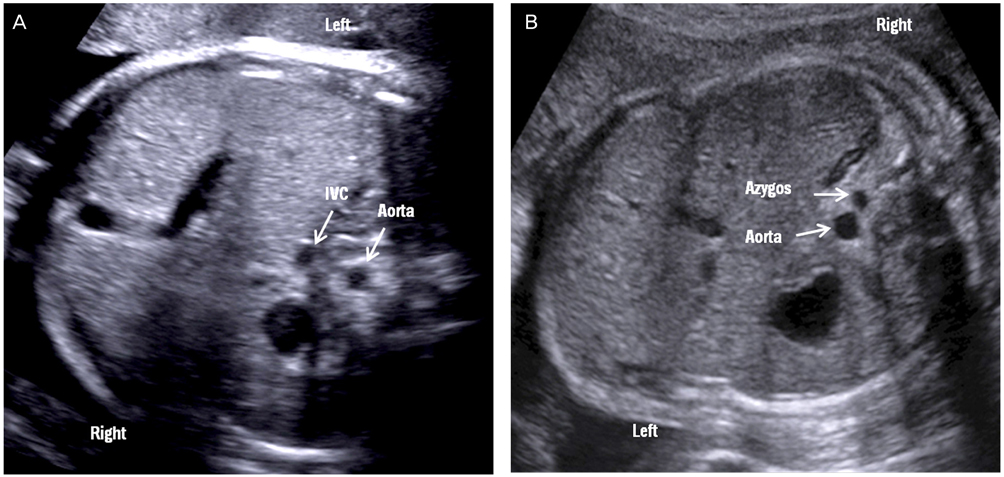
Of 43 fetuses with prenatally diagnosed right atrial isomerism (RAI), 40 cases were analyzed. The diagnostic accuracy was 93%. The main intracardiac anomalies in RAI were atrioventricular septal defect (AVSD), abnormal pulmonary venous connection, bilateral superior vena cava (BSVC), and pulmonary atresia. Among 28 live births, three infants were lost to follow up, and the overall survival rate was 60%. Of 37 fetuses with prenatally diagnosed left atrial isomerism (LAI), 35 were evaluated. The diagnostic accuracy was 97%. The main intracardiac anomalies in LAI were ventricular septal defect, BSVC, AVSD, double outlet right ventricle, and bradyarrhythmia. Among seven patients with bradyarrhythmia, only one showed a complete atrioventricular block. All fetuses had an interrupted inferior vena cava with azygous continuation. The overall survival rate was 90%.
CONCLUSION
Our study confirms the previous findings of fetal atrial isomerism. We also demonstrates a much lower prevalence of AVSD and complete heart block in LAI and a better survival rate in RAI. Although the postnatal outcomes for RAI were worse than those for LAI, successful postnatal surgery with active management improved the survival rate.
MeSH Terms
-
Atrioventricular Block
Bradycardia
Double Outlet Right Ventricle
Echocardiography
Fetus
Heart Block
Heart Defects, Congenital
Heart Septal Defects, Ventricular
Heterotaxy Syndrome
Humans
Infant
Isomerism*
Live Birth
Lost to Follow-Up
Prenatal Diagnosis*
Prevalence
Pulmonary Atresia
Retrospective Studies
Survival Rate
Vena Cava, Inferior
Vena Cava, Superior
Figure
Reference
-
1. Ho SY, Cook A, Anderson RH, Allan LD, Fagg N. Isomerism of the atrial appendages in the fetus. Pediatr Pathol. 1991; 11:589–608.2. Phoon CK, Villegas MD, Ursell PC, Silverman NH. Left atrial isomerism detected in fetal life. Am J Cardiol. 1996; 77:1083–1088.3. Atkinson DE, Drant S. Diagnosis of heterotaxy syndrome by fetal echocardiography. Am J Cardiol. 1998; 82:1147–1149.4. Lin JH, Chang CI, Wang JK, Wu MH, Shyu MK, Lee CN, et al. Intrauterine diagnosis of heterotaxy syndrome. Am Heart J. 2002; 143:1002–1008.5. Berg C, Geipel A, Smrcek J, Krapp M, Germer U, Kohl T, et al. Prenatal diagnosis of cardiosplenic syndromes: a 10-year experience. Ultrasound Obstet Gynecol. 2003; 22:451–459.6. Berg C, Geipel A, Kamil D, Knuppel M, Breuer J, Krapp M, et al. The syndrome of left isomerism: sonographic findings and outcome in prenatally diagnosed cases. J Ultrasound Med. 2005; 24:921–931.7. Lim JS, McCrindle BW, Smallhorn JF, Golding F, Caldarone CA, Taketazu M, et al. Clinical features, management, and outcome of children with fetal and postnatal diagnoses of isomerism syndromes. Circulation. 2005; 112:2454–2461.8. Taketazu M, Lougheed J, Yoo SJ, Lim JS, Hornberger LK. Spectrum of cardiovascular disease, accuracy of diagnosis, and outcome in fetal heterotaxy syndrome. Am J Cardiol. 2006; 97:720–724.9. Yan YL, Tan KB, Yeo GS. Right atrial isomerism: preponderance in Asian fetuses. Using the stomach-distance ratio as a possible diagnostic tool for prediction of right atrial isomerism. Ann Acad Med Singapore. 2008; 37:906–912.10. Pepes S, Zidere V, Allan LD. Prenatal diagnosis of left atrial isomerism. Heart. 2009; 95:1974–1977.11. Nakada K, Kawaguchi F, Wakisaka M, Nakada M, Enami T, Yamate N. Digestive tract disorders associated with asplenia/polysplenia syndrome. J Pediatr Surg. 1997; 32:91–94.12. Ticho BS, Goldstein AM, Van Praagh R. Extracardiac anomalies in the heterotaxy syndromes with focus on anomalies of midline-associated structures. Am J Cardiol. 2000; 85:729–734.13. Hsu JY, Chen SJ, Wang JK, Ni YH, Chang MH, Wu MH. Clinical implication of hiatal hernia in patients with right isomerism. Acta Paediatr. 2005; 94:1248–1252.14. Chang J, Brueckner M, Touloukian RJ. Intestinal rotation and fixation abnormalities in heterotaxia: early detection and management. J Pediatr Surg. 1993; 28:1281–1284.15. Vazquez J, Lopez Gutierrez JC, Gamez M, Lopez-Santamaria M, Murcia J, Larrauri J, et al. Biliary atresia and the polysplenia syndrome: its impact on final outcome. J Pediatr Surg. 1995; 30:485–487.16. Ruano R, Benachi A, Aubry MC, Bernard JP, Hameury F, Nihoul-Fekete C, et al. Prenatal sonographic diagnosis of congenital hiatal hernia. Prenat Diagn. 2004; 24:26–30.17. Simpson J, Zellweger H. Familial occurrence of Ivemark syndrome with splenic hypoplasia and asplenia in sibs. J Med Genet. 1973; 10:303–304.18. Rose V, Izukawa T, Moes CA. Syndromes of asplenia and polysplenia. A review of cardiac and non-cardiac malformations in 60 cases withspecial reference to diagnosis and prognosis. Br Heart J. 1975; 37:840–852.19. Zlotogora J, Elian E. Asplenia and polysplenia syndromes with abnormalities of lateralisation in a sibship. J Med Genet. 1981; 18:301–302.20. Eronen M, Kajantie E, Boldt T, Pitkanen O, Aittomaki K. Right atrial isomerism in four siblings. Pediatr Cardiol. 2004; 25:141–144.21. Kaasinen E, Aittomaki K, Eronen M, Vahteristo P, Karhu A, Mecklin JP, et al. Recessively inherited right atrial isomerism caused by mutations in growth/differentiation factor 1 (GDF1). Hum Mol Genet. 2010; 19:2747–2753.22. Celentano C, Malinger G, Rotmensch S, Gerboni S, Wolman Y, Glezerman M. Prenatal diagnosis of interrupted inferior vena cava as an isolated finding: a benign vascular malformation. Ultrasound Obstet Gynecol. 1999; 14:215–218.23. Bronshtein M, Khatib N, Blumenfeld Z. Prenatal diagnosis and outcome of isolated interrupted inferior vena cava. Am J Obstet Gynecol. 2010; 202:398.e1–398.e4.24. Freedom RM, Jaeggi ET, Lim JS, Anderson RH. Hearts with isomerism of the right atrial appendages: one of the worst forms of disease in 2005. Cardiol Young. 2005; 15:554–567.25. Waldman JD, Rosenthal A, Smith AL, Shurin S, Nadas AS. Sepsis and congenital asplenia. J Pediatr. 1977; 90:555–559.26. Ota N, Fujimoto Y, Murata M, Tosaka Y, Ide Y, Tachi M, et al. Improving outcomes of the surgical management of right atrial isomerism. Ann Thorac Surg. 2012; 93:832–838.27. Lee MY, Won HS. Technique of fetal echocardiography. Obstet Gynecol Sci. 2013; 56:217–226.28. Sheley RC, Nyberg DA, Kapur R. Azygous continuation of the interrupted inferior vena cava: a clue to prenatal diagnosis of the cardiosplenic syndromes. J Ultrasound Med. 1995; 14:381–387.