J Korean Fract Soc.
2014 Apr;27(2):151-156. 10.12671/jkfs.2014.27.2.151.
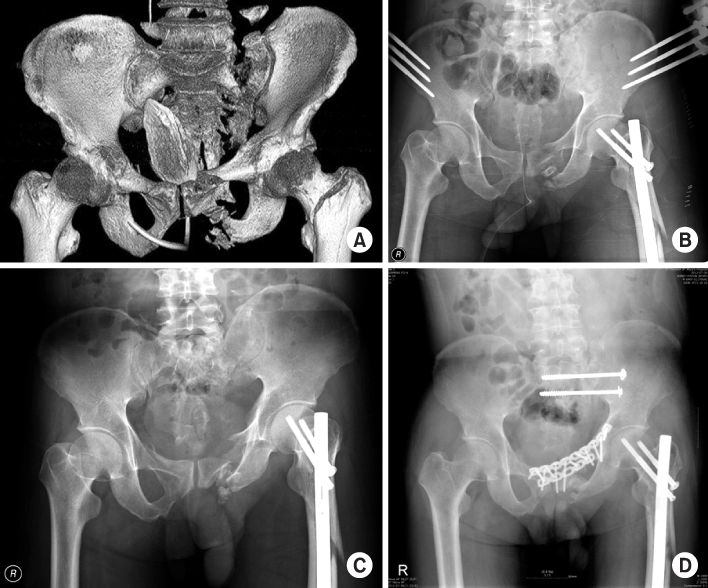
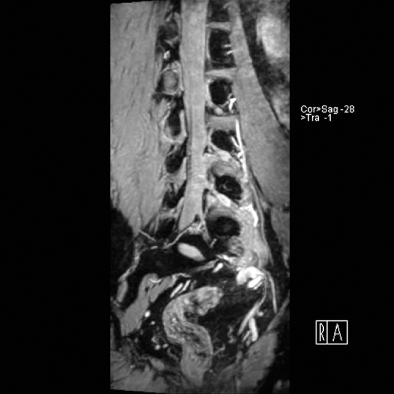
Surgical Correction and Osteosynthesis for Cranial Displaced Pelvic Nonunion: Technical Note and Two Cases Report Regarding Anterior Correction and Osteosynthesis Following Posterior Release
- Affiliations
-
- 1Department of Orthopedic Surgery, Daejeon St. Mary's Hospital, School of Medicine, The Catholic University of Korea, Daejeon, Korea. weonkim@hotmail.com
- KMID: 1703114
- DOI: http://doi.org/10.12671/jkfs.2014.27.2.151
Abstract
- Nonunion of an unstable pelvic fracture with cranial displacement pelvic surgery is technically difficult due to a large amount of bleeding and the risk of nerve damage. In addition, surgical correction of leg length discrepancy by reduction of a dislocated sacroiliac joint is in high demand. Nevertheless, when a patient is strongly disabled by a pelvic deformity, surgical correction may be necessary. Two patients with pelvic deformity were treated successfully by surgical correction and osteosynthesis.
MeSH Terms
Figure
Reference
-
1. Kellam JF, McMurtry RY, Paley D, Tile M. The unstable pelvic fracture. Operative treatment. Orthop Clin North Am. 1987; 18:25–41.2. Tile M. Pelvic ring fractures: should they be fixed? J Bone Joint Surg Br. 1988; 70:1–12.
Article3. van den Bosch EW, van Zwienen CM, van Vugt AB. Fluoroscopic positioning of sacroiliac screws in 88 patients. J Trauma. 2002; 53:44–48.
Article4. Matta JM, Dickson KF, Markovich GD. Surgical treatment of pelvic nonunions and malunions. Clin Orthop Relat Res. 1996; (329):199–206.
Article5. Mears DC, Velyvis J. Surgical reconstruction of late pelvic post-traumatic nonunion and malalignment. J Bone Joint Surg Br. 2003; 85:21–30.
Article6. Rousseau MA, Laude F, Lazennec JY, Saillant G, Catonné Y. Two-stage surgical procedure for treating pelvic malunions. Int Orthop. 2006; 30:338–341.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Testicular Necrosis after Ilioinguinal Approach for Pelvic Nonunion: A Case Report
- Osteosynthesis for Nonunion of the Lateral Condyle of the Humerus
- In Situ Late Metaphyseal Osteosynthesis for the Fractures of the Lateral Humeral Condyle in Children
- The Result of Osteosynthesis of Scaphoid with Matti-Russe Technique and Herbert Screw
- Humeral intramedullary nail bending following trauma: a case report