Yonsei Med J.
2013 Mar;54(2):396-402. 10.3349/ymj.2013.54.2.396.
Diagnostic Value and Prognostic Significance of Pleural C-Reactive Protein in Lung Cancer Patients with Malignant Pleural Effusions
- Affiliations
-
- 1Department of Laboratory Medicine, Institute of Wonkwang Medical Science, Wonkwang University School of Medicine, Iksan, Korea.
- 2Department of Internal Medicine, Institute of Wonkwang Medical Science, Wonkwang University School of Medicine, Iksan, Korea. kshryj@wonkwang.ac.kr
- 3Department of Obstetrics & Gynecology, Wonkwang University School of Medicine, Iksan, Korea.
- 4Department of Radiology, Wonkwang University School of Medicine, Iksan, Korea.
- KMID: 1503902
- DOI: http://doi.org/10.3349/ymj.2013.54.2.396
Abstract
- PURPOSE
C-reactive protein (CRP) has been implicated in various inflammatory and advanced malignant states. Increased serum CRP (s-CRP) levels have been shown to be associated with independent prognostic factors for survival in patients with advanced lung cancer. However, only few studies have focused on the role of CRP in pleural effusions. This study aimed to evaluate the diagnostic and prognostic value of pleural CRP (p-CRP) in lung cancer patients with malignant pleural effusion (MPE).
MATERIALS AND METHODS
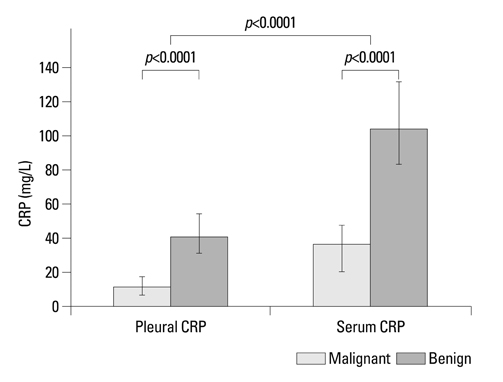
Pleural effusion (PE) samples were collected from patients with MPE (68 lung cancers; 12 extrathoracic tumors), and from 68 patients with various benign conditions (31 with pneumonia; 37 with tuberculosis). Concentrations of p- and s-CRP were measured by enzyme-linked immunosorbent assay. CRP level in pleural fluid and its association with survival were examined.
RESULTS
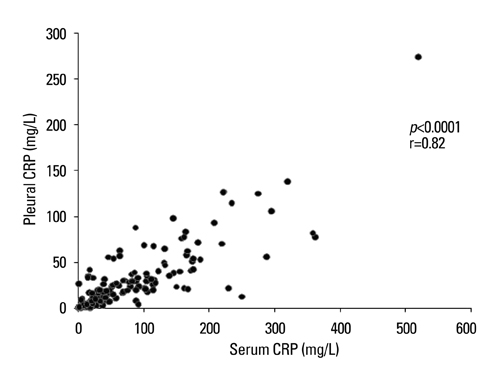
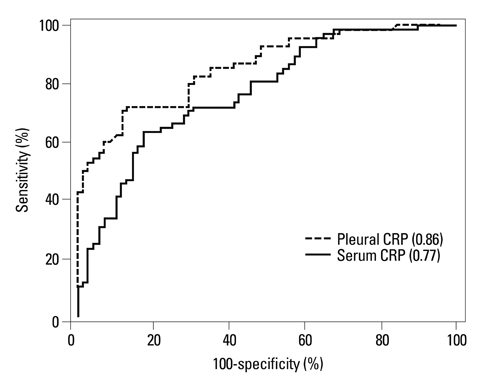
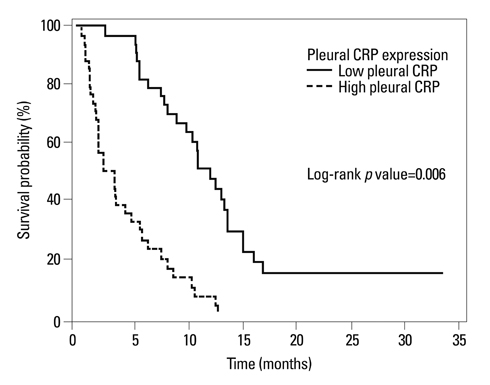
p-CRP levels correlated with s-CRP levels (r=0.82, p<0.0001). For the differential diagnosis of MPE and benign PE, the area under the receiver operating characteristic curve was greater for p-CRP (0.86) than for s-CRP (0.77). High p-CRP expression significantly correlated with shorter overall survival (p=0.006). P-CRP was independent prognostic factor significantly associated with overall survival on multivariated analysis (p=0.0001). The relative risk of death for lung cancer patients with high p-CRP levels was 3.909 (95% confidence interval, 2.000-7.639).
CONCLUSION
P-CRP is superior to s-CRP in determining pleural fluid etiology. Quantitative measurement of p-CRP might be a useful complementary diagnostic and prognostic test for lung cancer patients with MPE.
Keyword
MeSH Terms
Figure
Reference
-
1. Memon A, Zawadzki ZA. Malignant effusions: diagnostic evaluation and therapeutic strategy. Curr Probl Cancer. 1981. 5:1–30.
Article2. Postmus PE, Brambilla E, Chansky K, Crowley J, Goldstraw P, Patz EF Jr, et al. The IASLC Lung Cancer Staging Project: proposals for revision of the M descriptors in the forthcoming (seventh) edition of the TNM classification of lung cancer. J Thorac Oncol. 2007. 2:686–693.
Article3. Fiegl M, Massoner A, Steurer M, Grünewald K, Krugmann J, Hack R, et al. Improving tumor cell detection in pleural effusions by interphase cytogenetics. Cytometry B Clin Cytom. 2003. 55:60–62.
Article4. Ferrer J, Villarino MA, Encabo G, Felip E, Bermejo B, Vilà S, et al. Diagnostic utility of CYFRA 21-1, carcinoembryonic antigen, CA 125, neuron specific enolase, and squamous cell antigen level determinations in the serum and pleural fluid of patients with pleural effusions. Cancer. 1999. 86:1488–1495.
Article5. Miédougé M, Rouzaud P, Salama G, Pujazon MC, Vincent C, Mauduyt MA, et al. Evaluation of seven tumour markers in pleural fluid for the diagnosis of malignant effusions. Br J Cancer. 1999. 81:1059–1065.
Article6. Gu P, Huang G, Chen Y, Zhu C, Yuan J, Sheng S. Diagnostic utility of pleural fluid carcinoembryonic antigen and CYFRA 21-1 in patients with pleural effusion: a systematic review and meta-analysis. J Clin Lab Anal. 2007. 21:398–405.
Article7. Kim HJ, Shin KC, Lee JW, Kim KJ, Hong YH, Chung JH, et al. TNF-alpha in the pleural fluid for the differential diagnosis of tuberculous and malignant effusion. Tuberc Respir Dis. 2005. 59:625–630.
Article8. Liang QL, Shi HZ, Qin XJ, Liang XD, Jiang J, Yang HB. Diagnostic accuracy of tumour markers for malignant pleural effusion: a meta-analysis. Thorax. 2008. 63:35–41.
Article9. Duffy MJ. Role of tumor markers in patients with solid cancers: a critical review. Eur J Intern Med. 2007. 18:175–184.
Article10. Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002. 420:860–867.
Article11. Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008. 454:436–444.
Article12. Chiang AC, Massagué J. Molecular basis of metastasis. N Engl J Med. 2008. 359:2814–2823.
Article13. Mahmoud FA, Rivera NI. The role of C-reactive protein as a prognostic indicator in advanced cancer. Curr Oncol Rep. 2002. 4:250–255.
Article14. Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest. 2003. 111:1805–1812.
Article15. Korppi M, Heiskanen-Kosma T, Leinonen M. White blood cells, C-reactive protein and erythrocyte sedimentation rate in pneumococcal pneumonia in children. Eur Respir J. 1997. 10:1125–1129.
Article16. Smith RP, Lipworth BJ. C-reactive protein in simple community-acquired pneumonia. Chest. 1995. 107:1028–1031.
Article17. Castaño Vidriales JL, Amores Antequera C. Use of pleural fluid C-reactive protein in laboratory diagnosis of pleural effusions. Eur J Med. 1992. 1:201–207.18. Yilmaz Turay U, Yildirim Z, Türköz Y, Biber C, Erdoğan Y, Keyf AI, et al. Use of pleural fluid C-reactive protein in diagnosis of pleural effusions. Respir Med. 2000. 94:432–435.
Article19. Hara M, Matsuzaki Y, Shimuzu T, Tomita M, Ayabe T, Enomoto Y, et al. Preoperative serum C-reactive protein level in non-small cell lung cancer. Anticancer Res. 2007. 27:3001–3004.20. Pelliniemi TT, Irjala K, Mattila K, Pulkki K, Rajamäki A, Tienhaara A, et al. Finnish Leukemia Group. Immunoreactive interleukin-6 and acute phase proteins as prognostic factors in multiple myeloma. Blood. 1995. 85:765–771.
Article21. Jabs WJ, Busse M, Krüger S, Jocham D, Steinhoff J, Doehn C. Expression of C-reactive protein by renal cell carcinomas and unaffected surrounding renal tissue. Kidney Int. 2005. 68:2103–2110.
Article22. Nozoe T, Matsumata T, Kitamura M, Sugimachi K. Significance of preoperative elevation of serum C-reactive protein as an indicator for prognosis in colorectal cancer. Am J Surg. 1998. 176:335–338.
Article23. Hefler LA, Concin N, Hofstetter G, Marth C, Mustea A, Sehouli J, et al. Serum C-reactive protein as independent prognostic variable in patients with ovarian cancer. Clin Cancer Res. 2008. 14:710–714.
Article24. Hashimoto K, Ikeda Y, Korenaga D, Tanoue K, Hamatake M, Kawasaki K, et al. The impact of preoperative serum C-reactive protein on the prognosis of patients with hepatocellular carcinoma. Cancer. 2005. 103:1856–1864.
Article25. Light RW. Diagnostic principles in pleural disease. Eur Respir J. 1997. 10:476–481.
Article26. Papageorgiou E, Kostikas K, Kiropoulos T, Karetsi E, Mpatavanis G, Gourgoulianis KI. Increased oxidative stress in exudative pleural effusions: a new marker for the differentiation between exudates and transudates? Chest. 2005. 128:3291–3297.
Article27. Chierakul N, Kanitsap A, Chaiprasert A, Viriyataveekul R. A simple C-reactive protein measurement for the differentiation between tuberculous and malignant pleural effusion. Respirology. 2004. 9:66–69.
Article28. Kim DY, Lee YS, Ahn S, Chun YH, Lim KS. The usefulness of procalcitonin and C-reactive protein as early diagnostic markers of bacteremia in cancer patients with febrile neutropenia. Cancer Res Treat. 2011. 43:176–180.
Article29. Botana-Rial M, Casado-Rey P, Leiro-Fernández V, Andrade-Olivié M, Represas-Represas C, Fernández-Villar A. Validity of procalcitonin and C-reactive protein measurement when differentiating between benign and malignant pleural effusion. Clin Lab. 2011. 57:373–378.30. Heikkilä K, Ebrahim S, Lawlor DA. A systematic review of the association between circulating concentrations of C reactive protein and cancer. J Epidemiol Community Health. 2007. 61:824–833.
Article31. Scott HR, McMillan DC, Forrest LM, Brown DJ, McArdle CS, Milroy R. The systemic inflammatory response, weight loss, performance status and survival in patients with inoperable non-small cell lung cancer. Br J Cancer. 2002. 87:264–267.
Article32. Søyseth V, Benth JS, Stavem K. The association between hospitalisation for pneumonia and the diagnosis of lung cancer. Lung Cancer. 2007. 57:152–158.
Article33. Brundage MD, Davies D, Mackillop WJ. Prognostic factors in non-small cell lung cancer: a decade of progress. Chest. 2002. 122:1037–1057.34. Forrest LM, McMillan DC, McArdle CS, Angerson WJ, Dunlop DJ. Evaluation of cumulative prognostic scores based on the systemic inflammatory response in patients with inoperable non-small-cell lung cancer. Br J Cancer. 2003. 89:1028–1030.
Article35. O'Dowd C, McRae LA, McMillan DC, Kirk A, Milroy R. Elevated preoperative C-reactive protein predicts poor cancer specific survival in patients undergoing resection for non-small cell lung cancer. J Thorac Oncol. 2010. 5:988–992.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A study on lactic dehydrogenase activity of tuberculous pleural effusion
- A Study on Diagnostic Value of Lysozyme Activity in Various pleural effusions
- Vascular endothelial growth factor in malignant and tuberculous pleural effusions
- Diagnostic Value of Immunoglobulin in Malignant Pleural Effusions
- Comparison of Characteristics of Pleural Fluid and Blood in Mycoplasmal and Tuberculous Pleural Effusions