Clin Exp Otorhinolaryngol.
2008 Sep;1(3):166-170. 10.3342/ceo.2008.1.3.166.
Factors Related to Regional Recurrence in Early Stage Squamous Cell Carcinoma of the Oral Tongue
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. kimkwang@snu.ac.kr
- 2Department of Pathology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 1486089
- DOI: http://doi.org/10.3342/ceo.2008.1.3.166
Abstract
OBJECTIVES
This study analyzed various clinical and histopathologic factors for patients with early stage squamous cell carcinoma (SCC) of the oral tongue to define a high risk group for regional recurrence and finally to find out the indication of elective neck dissection (END).
METHODS
Retrospective chart review was performed for 63 patients with T1-T2N0 SCC of the oral tongue who underwent partial glossectomy with/without END. Clinical and histopathologic factors assessed were age, gender, clinical T stage, tumor cell differentiation, depth of invasion, pathologic nodal status, and intrinsic muscle involvement, perineural invasion, lymphovascular emboli and resection margin involvement.
RESULTS
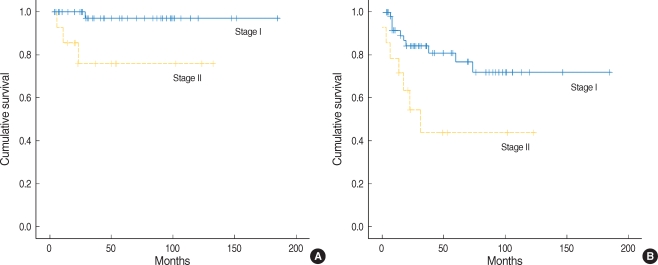
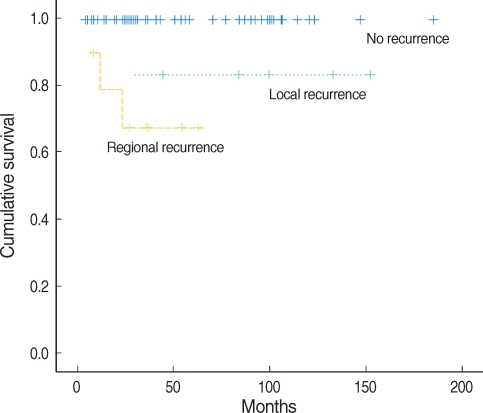
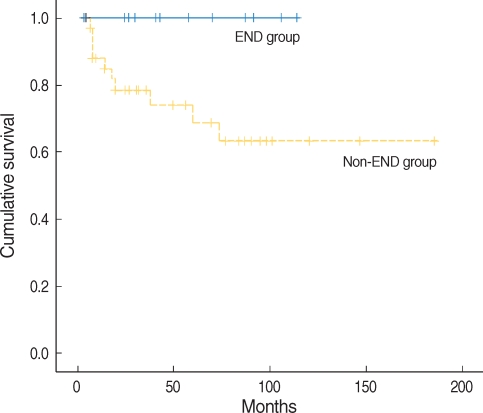
Five year overall survival rate was 97.1% in stage I and 76.2% in stage II, and 5-yr disease free survival rate was 76.7% in stage I and 43.5% in stage II. Rates of occult nodal metastasis in stage I and II were 15.4% and 42.9%, respectively. Overall regional recurrence rate was 15.9%, which consisted of 10.2% in stage I and 35.7% in stage II. The success rate of salvage treatment was 100% in stage I and 40% in stage II. Higher T stage, higher histologic grade, depth of invasion > or =3 mm, presence of intrinsic muscle involvement were significantly related to regional recurrence (P=0.035, P=0.011, P=0.016, P=0.009, respectively). In stage I, the non-END group (n=36) showed 13.9% of regional recurrence rate, while END group (n=13) did not have any regional recurrence (P=0.198). Five year disease free survival rate of END group was significantly higher than non-END group (100% and 68.7%, respectively, P=0.045).
CONCLUSION
We recommend to perform END in early stage SCC of the oral tongue if the primary tumor has T2 stage, and T1 stage with higher histologic grade, depth of invasion more than 3 mm, or presence of intrinsic muscle involvement.
MeSH Terms
Figure
Reference
-
1. Yuen AP, Wei WI, Wong YM, Tang KC. Elective neck dissection versus observation in the treatment of early oral tongue carcinoma. Head Neck. 1997; 10. 19(7):583–588. PMID: 9323146.
Article2. Haddadin KJ, Soutar DS, Oliver RJ, Webster MH, Robertson AG, MacDonald DG. Improved survival for patients with clinically T1/T2, N0 tongue tumors undergoing a prophylactic neck dissection. Head Neck. 1999; 9. 21(6):517–525. PMID: 10449667.
Article3. Keski-Säntti H, Atula T, Törnwall J, Koivunen P, Mäkitie A. Elective neck treatment versus observation in patients with T1/T2 N0 squamous cell carcinoma of oral tongue. Oral Oncol. 2006; 1. 42(1):96–101. PMID: 16256414.
Article4. Teichgraeber JF, Clairmont AA. The incidence of occult metastases for cancer of the oral tongue and floor of the mouth: treatment rationale. Head Neck Surg. 1984; 10. 7(1):15–21. PMID: 6490380.
Article5. Lim YC, Ahn JY, Koo BS, Lee JS, Chun JY, Park YM, et al. Occult lymph node metastasis in early oral tongue squamous cell carcinoma. Korean J Otolaryngol-Head Neck Surg. 2006; 4. 49(4):407–410.6. Yii NW, Patel SG, Rhys-Evans PH, Breach NM. Management of the N0 neck in early cancer of the oral tongue. Clin Otolaryngol Allied Sci. 1999; 2. 24(1):75–79. PMID: 10196656.
Article7. Spiro RH, Strong EW. Surgical treatment of cancer of the tongue. Surg Clin North Am. 1974; 8. 54(4):759–765. PMID: 4428313.
Article8. Kligerman J, Lima RA, Soares JR, Prado L, Dias FL, Freitas EQ, et al. Supraomohyoid neck dissection in the treatment of T1/T2 squamous cell carcinoma of oral cavity. Am J Surg. 1994; 11. 168(5):391–394. PMID: 7977957.
Article9. Kaya S, Yilmaz T, Gürsel B, Saraç S, Sennaroğlu L. The value of elective neck dissection in treatment of cancer of the tongue. Am J Otolaryngol. 2001; Jan–Feb. 22(1):59–64. PMID: 11172216.
Article10. Sparano A, Weinstein G, Chalian A, Yodul M, Weber R. Multivariate predictors of occult neck metastasis in early oral tongue cancer. Otolaryngol Head Neck Surg. 2004; 10. 131(4):472–476. PMID: 15467620.
Article11. Keski-Säntti H, Atula T, Tikka J, Hollmén J, Mäkitie AA, Leivo I. Predictive value of histopathologic parameters in early squamous cell carcinoma of oral tongue. Oral Oncol. 2007; 11. 43(10):1007–1013. PMID: 17306608.
Article12. Fakih AR, Rao RS, Borges AM, Patel AR. Elective versus therapeutic neck dissection in early carcinoma of the oral tongue. Am J Surg. 1989; 10. 158(4):309–313. PMID: 2802032.
Article13. Dias FL, Kligerman J, Matos de Sá G, Arcuri RA, Freitas EQ, Farias T, et al. Elective neck dissection versus observation in stage I squamous cell carcinomas of the tongue and floor of the mouth. Otolaryngol Head Neck Surg. 2001; 7. 125(1):23–29. PMID: 11458209.
Article14. Friedlander PL, Schantz SP, Shaha AR, Yu G, Shah JP. Squamous cell carcinoma of the tongue in young patients: a matched-pair analysis. Head Neck. 1998; 8. 20(5):363–368. PMID: 9663661.
Article15. Davidson BJ, Root WA, Trock BJ. Age and survival from squamous cell carcinoma of the oral tongue. Head Neck. 2001; 4. 23(4):273–279. PMID: 11400227.
Article16. Fukano H, Matsuura H, Hasegawa Y, Nakamura S. Depth of invasion as a predictive factor for cervical lymph node metastasis in tongue carcinoma. Head Neck. 1997; 5. 19(3):205–210. PMID: 9142520.
Article17. O'Brien CJ, Lauer CS, Fredricks S, Clifford AR, McNeil EB, Bagia JS, et al. Tumor thickness influences prognosis of T1 and T2 oral cavity cancer--but what thickness? Head Neck. 2003; 11. 25(11):937–945. PMID: 14603454.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Outcome of Squamous Cell Carcinoma of the Tongue in Young Patients: A Stage-Matched Comparative Analysis
- Expression of E-Cadherin and Matrix Metalloproteinase-2 in Squamous Cell Carcinoma of the Oral Tongue
- The characteristics and treatment results of squamous cell carcinomas of oral tongue
- A Case of Basaloid Squamous Cell Carcinoma Occurring in the Mobile Tongue
- Clinical Outcome of the Squamous Cell Carcinoma of Tongue: Experience of National Cancer Center