Clin Exp Otorhinolaryngol.
2010 Jun;3(2):107-109. 10.3342/ceo.2010.3.2.107.
Delayed Treatment of Zygomatic Tetrapod Fracture
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, Gachon University of Medicine & Science, Graduate School of Medicine, Incheon, Korea. eyik@gilhospital.com
- KMID: 1460598
- DOI: http://doi.org/10.3342/ceo.2010.3.2.107
Abstract
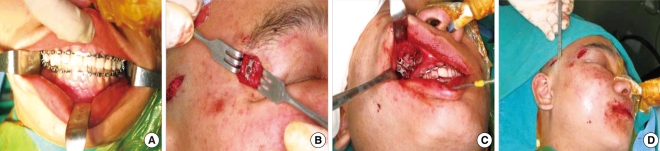
- Since maxillofacial injury is frequently accompanied by other diseases, its evaluation and treatment are open delayed. When the evaluation is delayed, the surgical treatment can be difficult or impossible. A 21-yr-old man presented with right facial swelling and deformity after injury. We planned immediate surgical repair for his right tetrapod fracture, but the operation was delayed for two months due to severe hyperthyroidism. During the operation, we reducted and fixed the deviated bone after refracture of the zygomatic arch with an osteotome to achieve mobility. The facial deformity and difficulty in mouth opening were improved after the operation. Even in the presence of accompanying fractures, early evaluation and proper management can prevent complications and achieve acceptable cosmetic outcomes in maxillofacial trauma patients. In patients with malunion of fracture sites, fixation after refracture using an osteotome can be a good treatment option for obtaining good mobility.
MeSH Terms
Figure
Reference
-
1. Moon JH, Kwon MS, Park SW, Kim YH, Han CY, Kwon JH, et al. Retrospective study on 527 patients with maxillofacial trauma: a 5-year experience. Korean J Otolaryngol - Head Neck Surg. 2004; 4. 47(4):362–367.2. Hogg NJ, Stewart TC, Armstrong JE, Girotti MJ. Epidemiology of maxillofacial injuries at trauma hospitals in Ontario, Canada, between 1992 and 1997. J Trauma. 2000; 9. 49(3):425–432. PMID: 11003318.
Article3. Nakamura T, Gross CW. Facial fractures: analysis of five year of experience. Arch Otolaryngol. 1973; 3. 97(3):288–290. PMID: 4696044.4. Bernstein L. Delayed management of facial fractures. Laryngoscope. 1970; 9. 80(9):1323–1341. PMID: 5470221.
Article5. Byrd HS, Hobar PC. Optimizing the management of secondary zygomatic fracture deformities: aesthetic and functional considerations. Clin Plast Surg. 1992; 1. 19(1):259–273. PMID: 1537223.6. Kim TH, Park HY, Park SC, Choi JS, Lim SC. A clinical analysis of facial bone fractures excluding nasal bone fractures. Korean J Otolaryngol - Head Neck Surg. 1997; 11. 40(11):1600–1608.7. Stanley RB Jr. Cummings CW, Fredrickson JM, Harker LA, Kraus CJ, Schuller DE, editors. Maxillofacial trauma. Otolaryngology-head and neck surgery. 1993. 2nd ed. St. Louis: Mosby Year Book;p. 374–402.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Classification and Clinical Analysis of Zygomatic Fractures
- Radiologic and Histological Study of Healing Process on Malunion Rat Model after Zygomatic Arch Fracture
- Intraoral Approach and K-Wire Fixation of Zygomatic Tripod Fractures
- Transcutaneous reduction and external bone fixation device for the treatment of zygomatic arch fracture
- K-wire Insertion Beneath Zygomatic Arch Under the Fluoroscope for Rigid Fixation of Zygomatic Arch Fracture