Clin Exp Otorhinolaryngol.
2010 Jun;3(2):96-101. 10.3342/ceo.2010.3.2.96.
Treatment Results of Major Salivary Gland Cancer by Surgery with or without Postoperative Radiation Therapy
- Affiliations
-
- 1Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. ahnyc@skku.edu
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1460596
- DOI: http://doi.org/10.3342/ceo.2010.3.2.96
Abstract
OBJECTIVES
This is to report treatment results of major salivary gland cancer by surgery with or without postoperative radiation therapy (PORT).
METHODS
Between March 1995 and January 2006, 94 patients with primary major salivary cancer underwent curative surgical resection at Samsung Medical Center. The parotid gland was the most commonly involved (73, 77.7%), followed by the submandibular and the sublingual. Neck dissection was added in 28 patients, and PORT was individually recommended to those with risk factors. Seventy-five (79.8%) patients received PORT. PORT volume included primary tumor bed and pathologically involved regional lymphatics, and no additional effort was made for elective nodal irradiation. The median total doses were 56.0 Gy to primary site and 58.7 Gy to regional lymphatics.
RESULTS
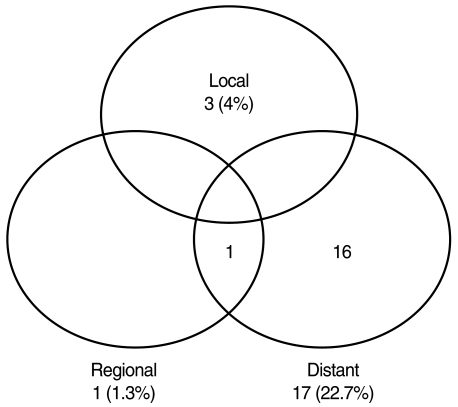
After median follow-up of 49 months, 21 patients had relapsed: 20 in PORT; and one in surgery alone group. As the first site of failure, distant metastasis was the most common (17 patients). Local recurrence occurred in three, and regional relapse in one. The lung was the most common site (10 patients), followed by the bone, and the brain. Five-yr disease free survival (DFS), local control, and overall survival (OS) rates were 74.4% and 94.7%, 96.0% and 100%, and 78.2% and 100% in PORT and surgery alone groups, respectively. On multivariate analysis, DFS was significantly affected by pN+ (hazard ratio [HR], 3.624; P=0.0319), while OS was by pN+ (HR, 7.138; P=0.0034) and perineural invasion (HR, 5.073; P=0.0187).
CONCLUSION
Based on our experience, the patients with early stage major salivary gland cancer with low risk can be effectively treated by surgery alone, and those who with risk factors can achieve excellent local and regional control by adding PORT. Omitting elective neck irradiation in patients with N0 disease seems a feasible strategy under accurate clinical evaluation. An effort is needed to decrease distant metastasis through further clinical trials.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Evaluation of Prognostic Factors for the Parotid Cancer Treated With Surgery and Postoperative Radiotherapy
Yong-Hyub Kim, Woong-Ki Chung, Jae-Uk Jeong, Ick Joon Cho, Mee Sun Yoon, Ju-Young Song, Taek-Keun Nam, Sung-Ja Ahn, Dong Hoon Lee, Tae Mi Yoon, Joon Kyoo Lee, Sang Chul Lim
Clin Exp Otorhinolaryngol. 2020;13(1):69-76. doi: 10.21053/ceo.2019.00388.
Reference
-
1. United States Cancer Statistics: 1999-2004 incidence and mortality web-based report [Internet]. National Cancer Institute. 2007. cited 2008 Nov 6. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute;Available from: http://www.cdc.gov/cancer/npcr/usc.2. Theriault C, Fitzpatrick PJ. Malignant parotid tumors: prognostic factors and optimum treatment. Am J Clin Oncol. 1986; 12. 9(6):510–516. PMID: 3788853.
Article3. Armstrong JG, Harrison LB, Spiro RH, Fass DE, Strong EW, Fuks ZY. Malignant tumors of major salivary gland origin: a matched-pair analysis of the role of combined surgery and postoperative radiotherapy. Arch Otolaryngol Head Neck Surg. 1990; 3. 116(3):290–293. PMID: 2306346.
Article4. North CA, Lee DJ, Piantadosi S, Zahurak M, Johns ME. Carcinoma of the major salivary glands treated by surgery or surgery plus postoperative radiotherapy. Int J Radiat Oncol Biol Phys. 1990; 6. 18(6):1319. 1326. PMID: 2115032.
Article5. Frankenthaler RA, Luna MA, Lee SS, Ang KK, Byers RM, Guillamondegui OM, et al. Prognostic variables in parotid gland cancer. Arch Otolaryngol Head Neck Surg. 1991; 11. 117(11):1251–1256. PMID: 1747227.
Article6. Spiro IJ, Wang CC, Montgomery WW. Carcinoma of the parotid gland: analysis of treatment results and patterns of failure after combined surgery and radiation therapy. Cancer. 1993; 5. 01. 71(9):2699–2705. PMID: 8467451.
Article7. Bell RB, Dierks EJ, Homer L, Potter BE. Management and outcome of patients with malignant salivary gland tumors. J Oral Maxillofac Surg. 2005; 7. 63(7):917–928. PMID: 16003616.
Article8. Terhaard CH, Lubsen H, Rasch CR, Levendag PC, Kaanders HH, Tjho-Heslinga RE, et al. The role of radiotherapy in the treatment of malignant salivary gland tumors. Int J Radiat Oncol Biol Phys. 2005; 1. 01. 61(1):103–111. PMID: 15629600.
Article9. Chen AM, Granchi PJ, Garcia J, Bucci MK, Fu KK, Eisele DW. Local-regional recurrence after surgery without postoperative irradiation for carcinomas of the major salivary glands: implications for adjuvant therapy. Int J Radiat Oncol Biol Phys. 2007; 3. 15. 67(4):982–987. PMID: 17241753.
Article10. Armstrong JG, Harrison LB, Thaler HT, Friedlander-Klar H, Fass DE, Zelefsky MJ, et al. The indications for elective treatment of the neck in cancer of the major salivary glands. Cancer. 1992; 2. 01. 69(3):615–619. PMID: 1730113.
Article11. Adams S, Baum RP, Stuckensen T, Bitter K, Hor G. Prospective comparison of 18F-FDG PET with conventional imaging modalities (CT, MRI, US) in lymph node staging of head and neck cancer. Eur J Nucl Med. 1998; 9. 25(9):1255–1260. PMID: 9724374.12. Nutting CM, Rowbottom CG, Cosgrove VP, Henk JM, Dearnaley DP, Robinson MH, et al. Optimisation of radiotherapy for carcinoma of the parotid gland: a comparison of conventional, three-dimensional conformal, and intensity-modulated techniques. Radiother Oncol. 2001; 8. 60(2):163–172. PMID: 11439211.
Article13. Garden AS, el-Naggar AK, Morrison WH, Callender DL, Ang KK, Peters LJ. Postoperative radiotherapy for malignant tumors of the parotid gland. Int J Radiat Oncol Biol Phys. 1997; 1. 01. 37(1):79–85. PMID: 9054880.
Article14. Storey MR, Garden AS, Morrison WH, Eicher SA, Schechter NR, Ang KK. Postoperative radiotherapy for malignant tumors of the submandibular gland. Int J Radiat Oncol Biol Phys. 2001; 11. 15. 51(4):952–958. PMID: 11704316.
Article15. Mendenhall WM, Morris CG, Amdur RJ, Werning JW, Villaret DB. Radiotherapy alone or combined with surgery for salivary gland carcinoma. Cancer. 2005; 6. 15. 103(12):2544–2550. PMID: 15880750.
Article16. Frankenthaler RA, Byers RM, Luna MA, Callender DL, Wolf P, Goepfert H. Predicting occult lymph node metastasis in parotid cancer. Arch Otolaryngol Head Neck Surg. 1993; 5. 119(5):517–520. PMID: 8484940.
Article17. Rodriguez-Cuevas S, Labastida S, Baena L, Gallegos F. Risk of nodal metastases from malignant salivary gland tumors related to tumor size and grade of malignancy. Eur Arch Otorhinolaryngol. 1995; 252(3):139–142. PMID: 7662346.
Article18. Regis De Brito Santos I, Kowalski LP, Cavalcante De Araujo V, Flavia Logullo A, Magrin J. Multivariate analysis of risk factors for neck metastases in surgically treated parotid carcinomas. Arch Otolaryngol Head Neck Surg. 2001; 1. 127(1):56–60. PMID: 11177015.
Article19. Bhattacharyya N, Fried MP. Nodal metastasis in major salivary gland cancer: predictive factors and effects on survival. Arch Otolaryngol Head Neck Surg. 2002; 8. 128(8):904–908. PMID: 12162768.20. Otsuka H, Graham MM, Kogame M, Nishitani H. The impact of FDG-PET in the management of patients with salivary gland malignancy. Ann Nucl Med. 2005; 12. 19(8):691–694. PMID: 16444995.
Article21. Cermik TF, Mavi A, Acikgoz G, Houseni M, Dadparvar S, Alavi A. FDG PET in detecting primary and recurrent malignant salivary gland tumors. Clin Nucl Med. 2007; 4. 32(4):286–291. PMID: 17413575.
Article22. Jeong HS, Chung MK, Son YI, Choi JY, Kim HJ, Ko YH, et al. Role of 18F-FDG PET/CT in management of high-grade salivary gland malignancies. J Nucl Med. 2007; 8. 48(8):1237–1244. PMID: 17631549.
Article23. Gurney TA, Eisele DW, Weinberg V, Shin E, Lee N. Adenoid cystic carcinoma of the major salivary glands treated with surgery and radiation. Laryngoscope. 2005; 7. 115(7):1278–1282. PMID: 15995521.
Article24. Terhaard CH, Lubsen H, Van der Tweel I, Hilgers FJ, Eijkenboom WM, Marres HA, et al. Salivary gland carcinoma: independent prognostic factors for locoregional control, distant metastases, and overall survival: results of the Dutch head and neck oncology cooperative group. Head Neck. 2004; 8. 26(8):681–692. PMID: 15287035.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Salivary Duct Carcinoma: 2 Case Reports
- A Case of Malignant Myoepithelioma in Parotid Gland
- A CASE OF CARCINOMA EX PLEOMORPHIC ADENOMA OF PALATE
- A Case of Multiple Sialoliths in Sublingual Gland Misdiagnosed as Sialoliths in Submandibular Gland
- A Case of Parotid Gland Salivary Fistula Treated by Tympanic Neurectomy