J Korean Soc Spine Surg.
2010 Jun;17(2):82-89. 10.4184/jkss.2010.17.2.82.
Risk Factors of Nonunion Demanding Surgical Treatment after Lumbar Posterolateral Fusion
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Dong-A University, Busan, Korea. gylee@dau.ac.kr
- KMID: 1459272
- DOI: http://doi.org/10.4184/jkss.2010.17.2.82
Abstract
- STUDY DESIGN: This is a retrospective study for radiographically and clinically assessing nonunion after lumbar spine fusion.
OBJECTIVES
We wanted to analyze the risk factors for nonunion that requires surgical treatment after lumbar spine fusion SUMMARY OF THE LITERATURE REVIEW: A diagnosis of the nonunion after lumbar spine fusion was made by using only the only radiologic images. The incidence of nonunion has been underreported because there are many asymptomatic patients.
MATERIALS AND METHODS
The plain X-ray films were evaluated for 1317 patients who could be followed up more than 1 year after lumbar fusion. Nonunion was diagnosed at 1 year after fusion by instability seen on the flexion-extension radiograph and the clinical findings like as sustained pain and local tenderness at the surgical site. The risk factors we reviewed included age, the number of levels fused, associated diseases, smoking, alcohol drinking, the initial diagnosis, a previous history of spinal operation, infection, a clear zone and malposition of pedicle screws and metal failure. The relations between nonunion and the factors mentioned above were analyzed.
RESULTS
Thirty-nine patients were diagnosed as having nonunion underwent reoperation and all had surgically confirmed nonunion. Smoking, infection and a previous history of spine operation had a significant influence on nonunion (p < 0.05). Clear zones persisting more than 1 year and metal failure also had a significant influence on nonunion (p < 0.05). Age, the number of fused levels, the initial diagnosis and alcohol drinking were not shown to influence the rate of nonunion (p < 0.05).
CONCLUSION
A through clinical and radiologic evaluation is essential to diagnose nonunion, and this should not be done according to the radiologic images only. Risk factors such as a previous history of spine operation, infection, smoking, the development of a clear zone and metal failure all showed a statistically significant influence on nonunion. Additionally, preoperative and postoperative evaluation of these parameters is needed to achieve bone union.
Keyword
MeSH Terms
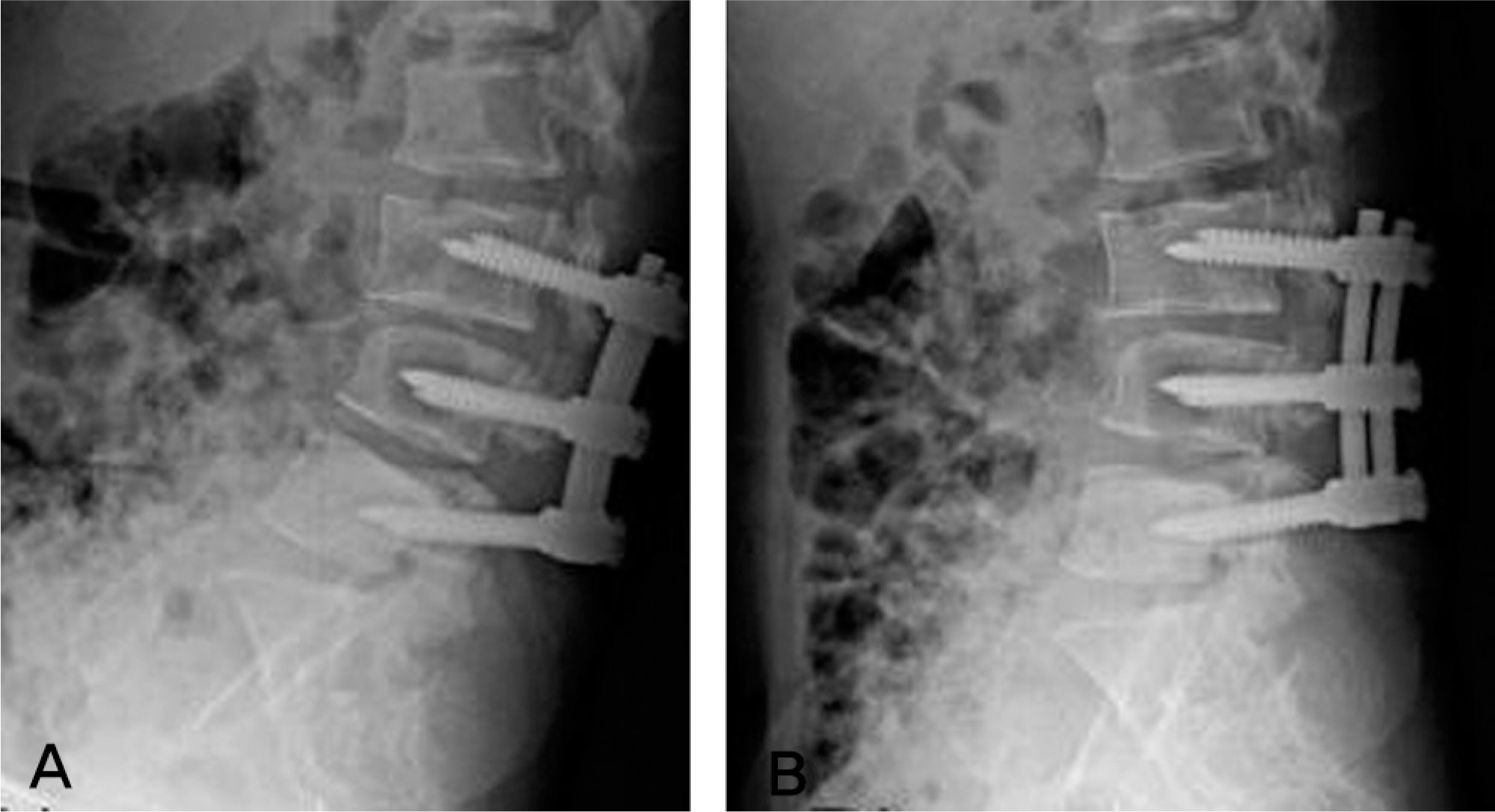
Figure
Reference
-
1.Cohen DB., Chotivichit A., Fujita T, et al. Pseudoarthrosis repair. Autogenous Iliac Crest Versus Femoral Ring Allograf. Clin Orthop. 2000. 371:46–55.2.Fischgrund JS., Mackay M., Herkowitz HN., Brower R., Montgomery DM., Kurz LT. 1997 Volvo Award winner in clinical studies. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine. 1997. 22:2807–12.3.Weinstein MA., McCabe JP., Cammisa FP Jr. Postoperative spinal wound infection: a review of 2,391 consecutive index procedures. J Spinal Disord. 2000. 13:422–6.
Article4.Lee C., Dorcil J., Radomisli TE. Nonunion of the spine: A Review. Clin Orthop Relat Res. 2004. 419:71–5.5.Albert TJ., Pinto M., Denis F. Management of symptomatic lumbar pseudoarthrosis with anteriorposterior fusion. A functional and radiographic outcome study. Spine. 2000. 25:123–9.6.Hilibrand AS., Dina TS. The use of diagnostic imaging to assess spinal arthrodesis. Orthop Clin North Am. 1998. 29:591–601.
Article7.Rawlins BA., Michesen CB. Failed lumbosacral fusions: state of the art review. Spine. 1994. 8:563–71.8.Steib JP., Bogorin I., Brax M., Lang G. Results of lumbar and lumbosacral fusion: clinical and radiological correlations in 113 cases reviewed at 3.8 years. Rev Chir Orthop Reparatrice Appar Mot. 2000. 86:127–35.9.Mok JM., Cloyd JM., Bradford DS, et al. Reoperation after primary fusion for adult spinal deformity: rate, reason, and timing. Spine. 2009. 34:832–9.10.Tokuhashi Y., Matsuzaki H., Oda H., Uei H. Clinical course and significance of the clear zone around the pedicle screws in the lumbar degenerative disease. Spine. 2008. 8:903–8.
Article11.Tokuhashi Y., Nishimura T., Matsuzaki Y. Clinical results of more than 10 years after poste rolateral fusion with pedicle screw fixation for degenerative lumbar spondylolisthesis. Spine. 2004. 17:185–92.12.Roy-Camille R., Saillant G., Mazel C. Plating of thoracic, thoracolumbar, and lumbar injuries with pedicle screw plates. Orthop Clin North Am. 1986. 17:147–59.
Article13.Okuyama K., Abe E., Suzuki T., Tamura Y., Chiba M., Sato K. Posterior lumbar interbody fusion. A retrospective study of complications after facet joint excision and pedicle screw fixation in 148 cases. Acta Orthop Scand. 1999. 70:329–34.
Article14.Kant AP., Daum WJ., Dean SM., Uchida T. Evaluation of lumbar spine fusion. Plain radiographs versus direct surgical exploration and observation. Spine. 1995. 21:2313–7.15.Kim KT., Suk KS., Lee SH., Kim JM. Revision arthrodesis after lumbar fusion in degenerative lumbar disease. J Kor Orthop Assoc. 2003. 38:659–64.
Article16.Selby DK., Henderson RJ., Blumenthal S., Dossett D. Anterior lumbar fusion. White AH, Rothman RH, Ray CD, editors. Lumbar spine surgery: techniques and complications. St. Louis: C.V. Mosby;1987. p. 112–32.17.Cleveland M., Bosworth DM., Frederick R, et al. Pseudarthrosis in the lumbosacral spine. J Bone Joint Surg Am. 1947. 30:302–12.
Article18.Brown CW., Orme TJ., Richardson HD. The rate of pseudarthrosis (surgical nonunion) in patients who are smokers and patients who are nonsmokers: A comparison study. Spine. 1986. 11:942–3.
Article19.Hadley MN., Reddy SV. Smoking and the human vertebral column: a review of the impact of cigarette use on vertebral bone metabolism and spinal fusion. Neurosurgery. 1997. 41:116–24.
Article20.Fritzell P., Hä gg O., Wessberg P., Nordwall A. Swedish Lumbar Spine Study Group. 2001 Volvo Award Winner in Clinical Studies: Lumbar fusion versus nonsurgical treatment for chronic low back pain: a multicenter randomized controlled trial from the Swedish Lumbar Spine Study Group. Spine. 2001. 26:2521–32.21.Brox JI., Sørensen R., Friis A, et al. Randomized clinical trial of lumbar instrumented fusion and cognitive intervention and exercises in patients with chronic low back pain and disc degeneration. Spine. 2003. 28:1913–21.22.Raizman NM., O'Brien JR., Poehling-Monaghan KL., Yu WD. Pseudarthrosis of the spine. J Am Acad Orthop Surg. 2009. 17:494–503.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison between Posterior Lumbar Interbody Fusion with Pedicle Screw Fixation and Posterolateral Fusion with Pedicle Screw Fixation in Spondylolytic Spondylolisthesis in Adults
- The Importance of Proximal Fusion Level Selection for Outcomes of Multi-Level Lumbar Posterolateral Fusion
- Transforaminal Lumbar Interbody Fusion for the Treatment of Nonunion after Posterolateral Lumbar Fusion
- A Comparison of Posterolateral and Posterior Interbody Fusion in the Surgical Treatment of Lumbar Spondylolisthesis
- The Result of the Posterolateral Fusion with Knodt Rod and without Knodt Rod in Spondylolysis and Spondylolisthesis of the Lumbar Spine