J Cardiovasc Ultrasound.
2010 Mar;18(1):28-30. 10.4250/jcu.2010.18.1.28.
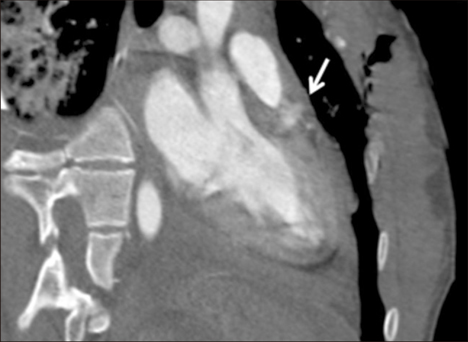
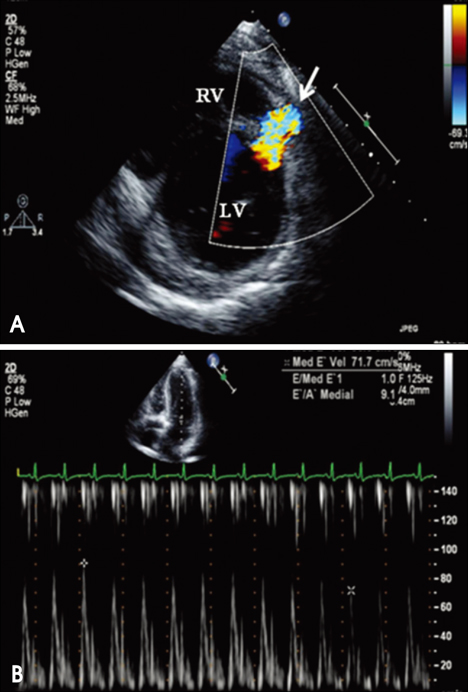
Delayed Diagnosis of Traumatic Ventricular Septal Defect in Penetrating Chest Injury: Small Evidence on Echocardiography Makes Big Difference
- Affiliations
-
- 1Cardiovascular Center, Seoul National University Hospital, Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. cardiman@medimail.co.kr
- KMID: 1457203
- DOI: http://doi.org/10.4250/jcu.2010.18.1.28
Abstract
- Cardiac trauma from penetrating chest injury is a life-threatening condition. It was reported that < 10% of patients arrives at the emergency department alive. Penetrating chest injury can cause serious damage in more than 1 cardiac structure, including myocardial lacerations, ventricular septal defect (VSD), fistula between aorta and right cardiac chamber and valves. The presence of pericardial effusion (even a small amount) on the initial echocardiography might be the only clue to serious cardiac damage in the absence of definite evidence of anatomical defect in heart. We here present a case, in which clear diagnosis of VSD and pseudoaneurysmal formation was delayed a few days after penetrating chest injury due to the lack of anatomical evidence of damage.
MeSH Terms
Figure
Reference
-
1. Campbell NC, Thomson SR, Muckart DJ, Meumann CM, Van Middelkoop I, Botha JB. Review of 1198 cases of penetrating cardiac trauma. Br J Surg. 1997. 84:1737–1740.
Article2. Mulder DG. Stab Wound of the Heart. Ann Surg. 1964. 160:287–291.
Article3. Karrel R, Shaffer MA, Franaszek JB. Emergency diagnosis, resuscitation, and treatment of acute penetrating cardiac trauma. Ann Emerg Med. 1982. 11:504–517.
Article4. Cowgill LD, Campbell DN, Clarke DR, Hammermeister K, Groves BM, Woelfel GF. Ventricular septal defect due to nonpenetrating chest trauma: use of the intra-aortic balloon pump. J Trauma. 1987. 27:1087–1090.5. Bromberg BI, Mazziotti MV, Canter CE, Spray TL, Strauss AW, Foglia RP. Recognition and management of nonpenetrating cardiac trauma in children. J Pediatr. 1996. 128:536–541.
Article6. Rollins MD, Koehler RP, Stevens MH, Walsh KJ, Doty DB, Price RS, Allen TL. Traumatic ventricular septal defect: case report and review of the English literature since 1970. J Trauma. 2005. 58:175–180.
Article7. Hee-Jung Yun, Seung-Won Jin, Young-Yong Ahn, Joo-Hyun Lee, Young-Joo Kim, Jong-Beom Kwan, Ho-Joong Youn, Keon Park, Jun-Chul Park, Chi-Kyung Kim, Jae-Hyung Kim, Soon-Jo Hong, Kyu-Bo Choi. A case of isolated ventricular septal rupture following non-penetrating chest trauma. J Korean Soc Echocardiogr. 2001. 9:157–156.
Article8. Rotman M, Peter RH, Sealy WC, Morris JJ Jr. Traumatic ventricular septal defect secondary to nonpenetrating chest trauma. Am J Med. 1970. 48:127–131.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- One Stage Repair of Traumatic Ventricular Septal Defect and Mitral Regurgitation
- A Knife Penetrating the Right Ventricle, Interventricular Septum, and 2 Valves: A Case Report
- A Case of Traumatic Ventricular Septal Defect Secondary to Nonpenetrating Chest Trauma
- Traumatic ventricular septal defect in a 4-year-old boy after blunt chest injury
- Surgical Treatment of Traumatic Ventricular Septal Defect by Penetrating Chest Injury