Korean J Obstet Gynecol.
2010 Oct;53(10):927-933. 10.5468/kjog.2010.53.10.927.
Learning curves of total laparoscopic hysterectomies in three gynecologists
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Guro Hospital, Korea University College of Medicine, Seoul, Korea. shinjh@korea.ac.kr
- KMID: 1453758
- DOI: http://doi.org/10.5468/kjog.2010.53.10.927
Abstract
OBJECTIVE
Total laparoscopic hysterectomy (TLH) is becoming more commonly used as an alternative to traditional abdominal hysterectomy and Analyzing the turning point of a learning curve can be useful in planning training programs. This study was to define the average turning point of a learning curve of TLH by comparing three separate gynecologists in one institute.
METHODS
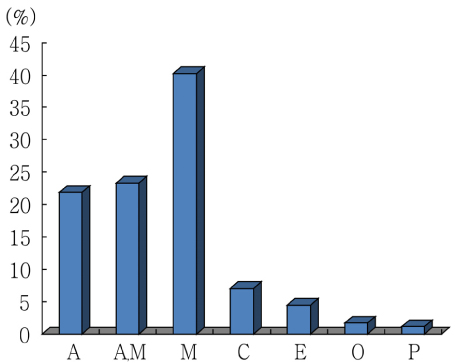
Retrospective analysis of the first 140 consecutive cases of TLH performed by three separate gynecologists A, B, and C. Patients of each gynecologist were divided into 7 equal groups of 20 operations classed chronologically. Patient's age, uterus weight, operation time and pre-post operative hemoglobin difference of the three gynecologists were compared. Operation time and pre-post operative hemoglobin difference were evaluated to build learning curves for each gynecologist.
RESULTS
Learning curve built by operation time showed turning point after 80~100 cases in all three gynecologists. Learning curve built by pre-post operative hemoglobin difference did not show a decreasing pattern. There were no statistical differences in patient's age and pre-post operative hemoglobin difference between the three gynecologists. However, mean uterine weight of gynecologist C was significantly lighter than that of gynecologist A and B. Operation time was significantly longer in cases by gynecologist C than in cases by A and B.
CONCLUSION
At least 80~100 cases of experience in TLH is needed for a gynecologist to reach the turning point of the learning curve. This result can be used as a guide to the training program of TLH.
Keyword
MeSH Terms
Figure
Reference
-
1. Berek JS, Novak E. Berek & Novak's gynecology. 2007. 14th ed. Philadelphia: Lippincott Williams & Wilkins.2. Garrett AJ, Nascimento MC, Nicklin JL, Perrin LC, Obermair A. Total laparoscopic hysterectomy: the Brisbane learning curve. Aust N Z J Obstet Gynaecol. 2007. 47:65–69.3. Gwon YI, Yoo YO, Lee HJ, Park TC, Shin JW, Lee JM, et al. Total laparoscopic hysterectomy: a review of 300 cases. Korean J Obstet Gynecol. 2001. 44:139–144.4. Kim S, Son H, Park S, Chung JY, Kim H, Lee Y, et al. The clinical studies on 600 cases of total laparoscopic hysterectomy (TLH). Korean J Obstet Gynecol. 2006. 49:2356–2361.5. Kim SH, Kim DH, Pai DH. Comparison of CISH with TLH, LAVH. Korean J Obstet Gynecol. 1996. 39:1263–1272.6. Kim YJ, Ha BS, Lee BD, Lee JK, Son YS, Chough YW. Total laparoscopic hysterectomy (TLH): a clinical review of 300 cases. Korean J Obstet Gynecol. 2002. 45:292–297.7. Kim YS, Lee HS, Kwon SY, Eun MN, Lee GS, Park YS, et al. Simple total laparoscopic hysterectomy: a clinical evaluation of 312 cases. Korean J Obstet Gynecol. 2004. 47:10–15.8. Perino A, Cucinella G, Venezia R, Castelli A, Cittadini E. Total laparoscopic hysterectomy versus total abdominal hysterectomy: an assessment of the learning curve in a prospective randomized study. Hum Reprod. 1999. 14:2996–2999.9. Kolkman W, Engels LE, Smeets MJ, Jansen FW. Teach the teachers: an observational study on mentor traineeship in gynecological laparoscopic surgery. Gynecol Obstet Invest. 2007. 64:1–7.10. Altgassen C, Michels W, Schneider A. Learning laparoscopic-assisted hysterectomy. Obstet Gynecol. 2004. 104:308–313.11. Choi DH, Jeong WK, Lim SW, Chung TS, Park JI, Lim SB, et al. Learning curves for laparoscopic sigmoidectomy used to manage curable sigmoid colon cancer: single-institute, three-surgeon experience. Surg Endosc. 2009. 23:622–628.12. Ramsay CR, Wallace SA, Garthwaite PH, Monk AF, Russell IT, Grant AM. Assessing the learning curve effect in health technologies. Lessons from the nonclinical literature. Int J Technol Assess Health Care. 2002. 18:1–10.13. Harkki-Siren P, Sjoberg J. Evaluation and the learning curve of the first one hundred laparoscopic hysterectomies. Acta Obstet Gynecol Scand. 1995. 74:638–641.14. Nezhat C, Nezhat F, Admon D, Nezhat AA. Proposed classification of hysterectomies involving laparoscopy. J Am Assoc Gynecol Laparosc. 1995. 2:427–429.15. Lee KH, Park YS, Kang KC. Study on repairing method of vaginal cuff in total laparoscopic hysterectomy. Korean J Obstet Gynecol. 2000. 43:670–674.16. Olive DL, Parker WH, Cooper JM, Levine RL. The AAGL classification system for laparoscopic hysterectomy. Classification committee of the American Association of Gynecologic Laparoscopists. J Am Assoc Gynecol Laparosc. 2000. 7:9–15.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Total Laparoscopic Hysterectomy using Modified Bae's Uterine Elevator
- Learning Curve for Laparoscopic Colorectal Surgery: Hand Assisted Laparoscopic Surgery (HALS) versus Conventional Laparoscopic Surgery (CLS)
- The Learning Curve by Varied Operative Procedures in Laparoscopic Colorectal Surgery
- Learning Curve and Clinicopathologic Analysis in Transperitoneal Laparoscopic Adrenalectomy; Performed by a Single Young Surgeon with No Experience of Open Adrenalectomy
- Total laparoscopic hysterectomy versus da Vinci robotic hysterectomy: is using the robot beneficial?