J Korean Bone Joint Tumor Soc.
2011 Dec;17(2):100-105. 10.5292/jkbjts.2011.17.2.100.
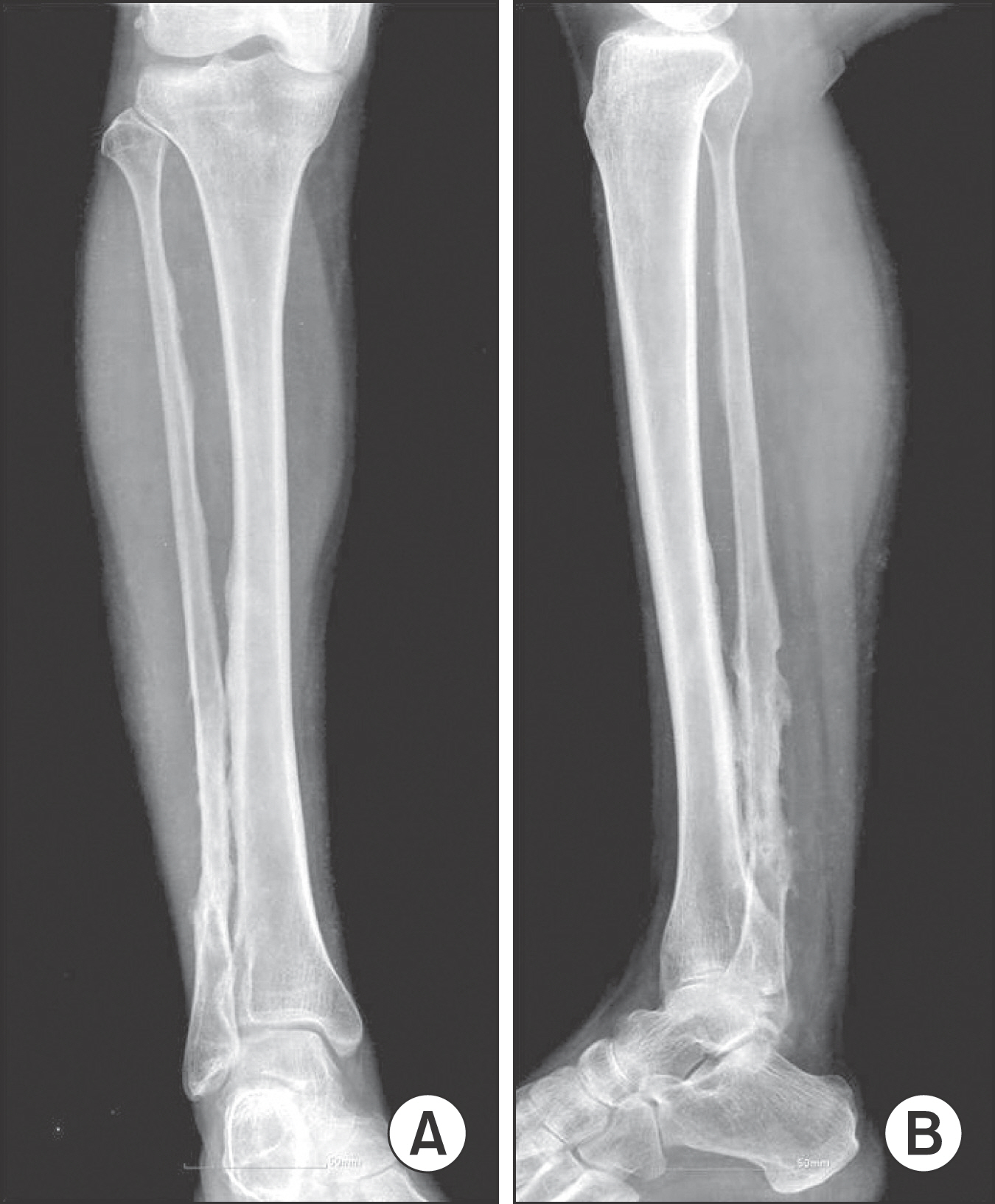
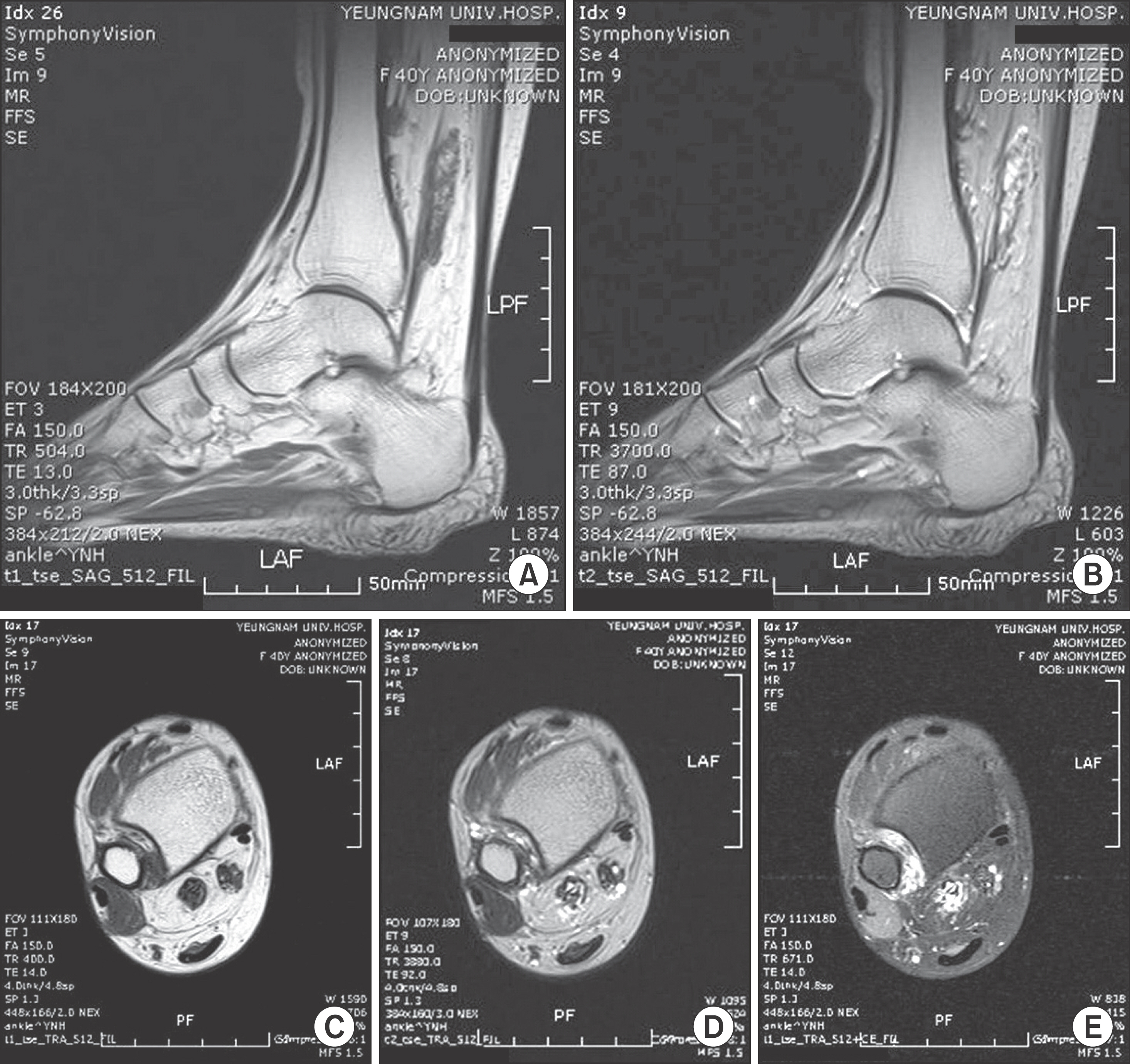
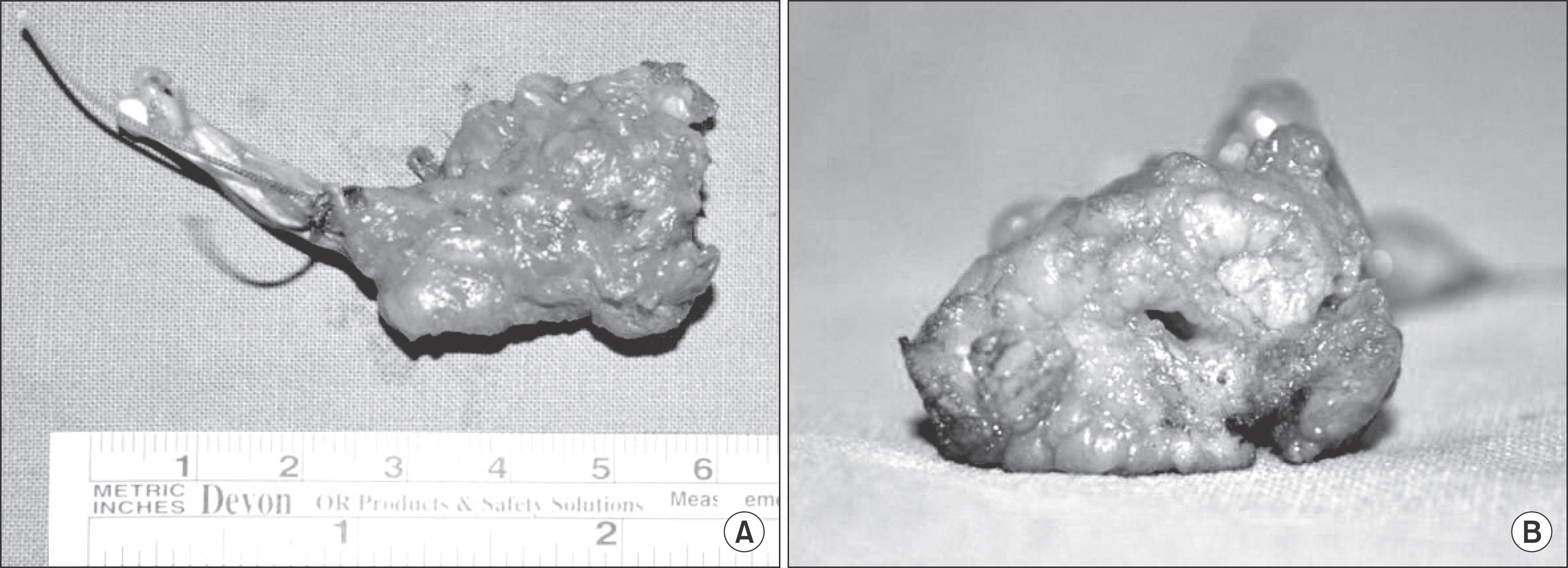
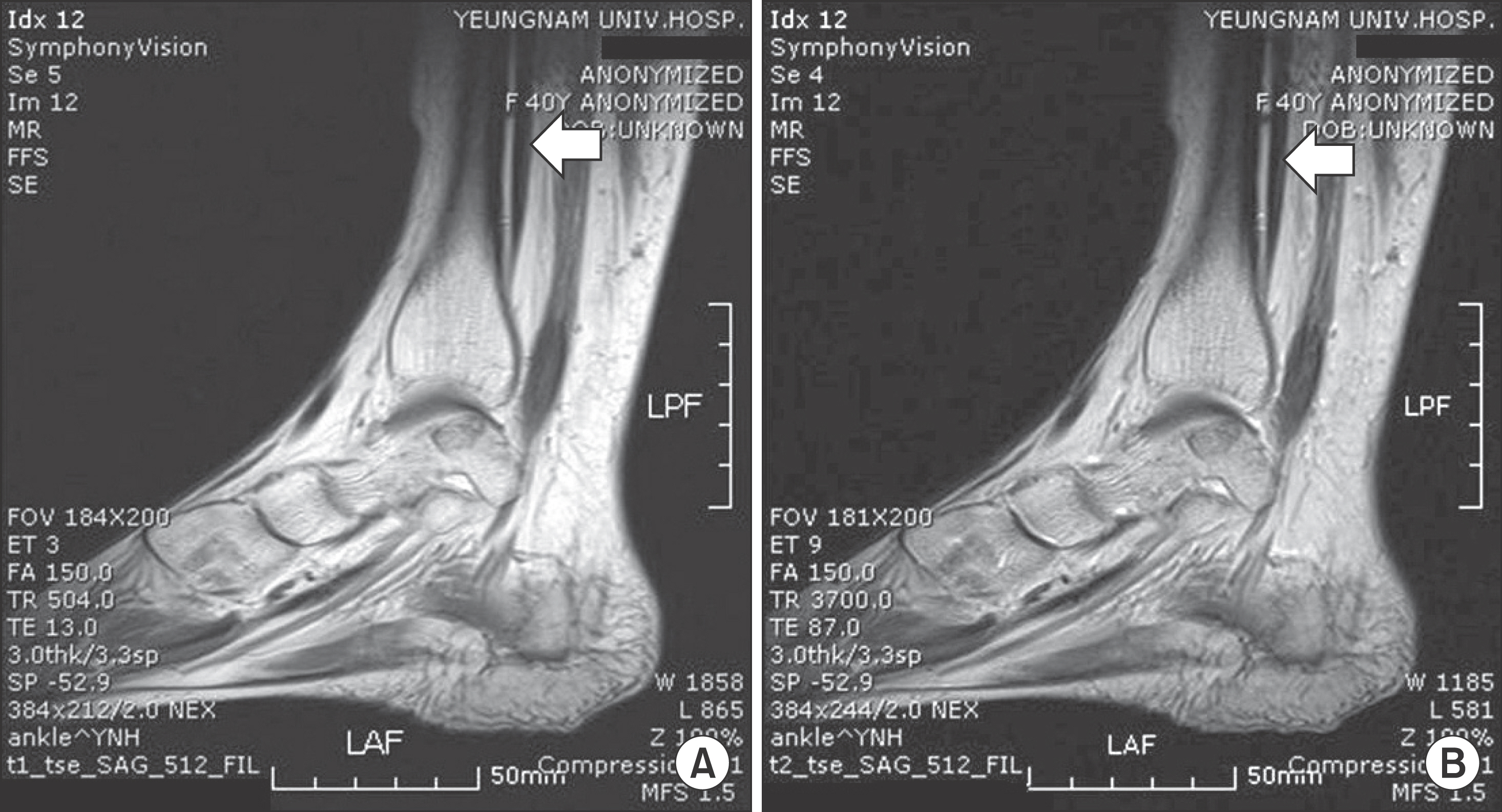
Vascular Malformation of Flexor Hallucis Longus Muscle Associated with a Flexion Deformities of Toes: A Case Report
- Affiliations
-
- 1Department of Orthopaedic Surgery, Yeungnam University College of Medicine, Daegu, Korea. shinds@med.yu.ac.kr
- KMID: 1444797
- DOI: http://doi.org/10.5292/jkbjts.2011.17.2.100
Abstract
- Vascular malformations may typically present with palpable mass that can be either asymptomatic or can present with symptoms including swelling and pain. On rare occasions, vascular malformation of muscle may produce joint deformities caused by contracture of the involved muscle. When vascular malformation involves the flexor muscle of the leg, ankle equinus deformity may occur. However, there are no reports of toe deformities secondary to intermuscular or intramuscular vascular malformations of flexor muscles of toe. Thus, we report a case of vascular malformation of flexor hallucis longus muscle with flexion contracture of toes in a 40-years-old woman who was treated with surgical excision.
MeSH Terms
Figure
Reference
-
References
1. Carpenter EB, Strawn LM. Hemangiomatosis of the ulna and flexor muscles of the forearm with secondary flexion contracture of the wrist and hand. A case report. J Bone Joint Surg Am. 1963; 45:1472–8.2. Domb BG, Khanna AJ, Mitchell SE, Frassica FJ. Toe-walking attributable to venous malformation of the calf muscle. Clin Orthop Relat Res. 2004; 420:225–9.
Article3. Lee SH, Shin KH, Yang WI, Suh JS, Hahn SB. Surgical treatment of hemangioma in the extremities. J Korean Orthop Assoc. 2004; 39:215–21.
Article4. Sutherland AD. Equinus deformity due to haemangioma of calf muscle. J Bone Joint Surg Br. 1975; 57:104–5.
Article5. Enzinger FM, Weiss SW. Soft tissue tumors. 4th ed.St Louis: Mosby;2001. p. 837–87.6. Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg. 1982; 69:412–22.7. Rogalski R, Hensinger R, Loder R. Vascular abnormalities of the extremities: Clinical findings and management. J Pediatr Orthop. 1993; 13:9–14.8. Wild AT, Raab P, Krauspe R. Hemangioma of skeletal muscle. Arch Orthop Trauma Surg. 2000; 120:139–43.
Article9. Hawnaur JM, Whitehouse RW, Jenkins JP, Isherwood I. Musculoskeletal haemangiomas: comparison of MRI with CT. Skeletal Radiol. 1990; 19:251–8.
Article10. Klemme WR, James P, Skinner SR. Latent onset unilateral toe-walking secondary to hemangioma of the gastrocnemius. J Pediatr Orthop. 1994; 14:773–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tendonitis of the Flexor Hallucis Longus with Triggering of the Great Toe: A Case Report
- Management of Checkrein Deformity
- Trigger Toe in Soccer Player: A Case Report
- Checkrein deformity of the lesser toes following comminuted fracture of calcaneus : A Case Report
- The Checkrein Deformity of Extensor Hallucis Longus Tendon and Extensor Retinaculum Syndrome with Deep Peroneal Nerve Entrapment after Triplane Fracture: A Case Report