J Korean Neurosurg Soc.
2012 Feb;51(2):81-85. 10.3340/jkns.2012.51.2.81.
The Effect of Body Mass Index on Intra-Abdominal Pressure and Blood Loss in Lumbar Spine Surgery
- Affiliations
-
- 1Department of Neurosurgery, Medical Research Institute, Pusan National University Hospital, Busan, Korea.
- 2Department of Neurosurgery, Yangsan Pusan National University Hospital, Yangsan, Korea. md6576@naver.com
- KMID: 1441414
- DOI: http://doi.org/10.3340/jkns.2012.51.2.81
Abstract
OBJECTIVE
The purpose of this prospective study was to evaluate the effects of body mass index (BMI) on intra-abdominal pressure (IAP) and intraoperative blood loss (IBL) during lumbar spinal surgery.
METHODS
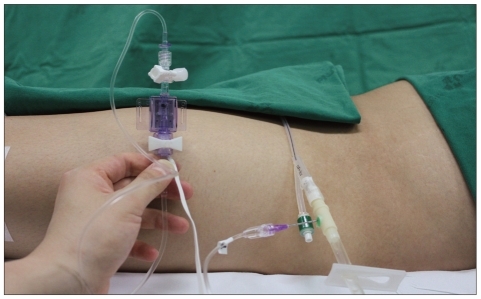
Thirty patients scheduled for single level posterior lumbar interbody fusion were allocated equally to a normal group (Group 1, BMI;18.5-22.9 kg/m2), an overweight group (Group 2, BMI; 23-24.9 kg/m2), and an obese group (Group 3, BMI; 25.0-29.9 kg/m2) according to BMI. IAP was measured using a urinary bladder catheter; 1) supine after anesthesia induction, 2) prone at skin incision, 3) prone at the end of surgery. In addition, IBL was also measured in the three groups.
RESULTS
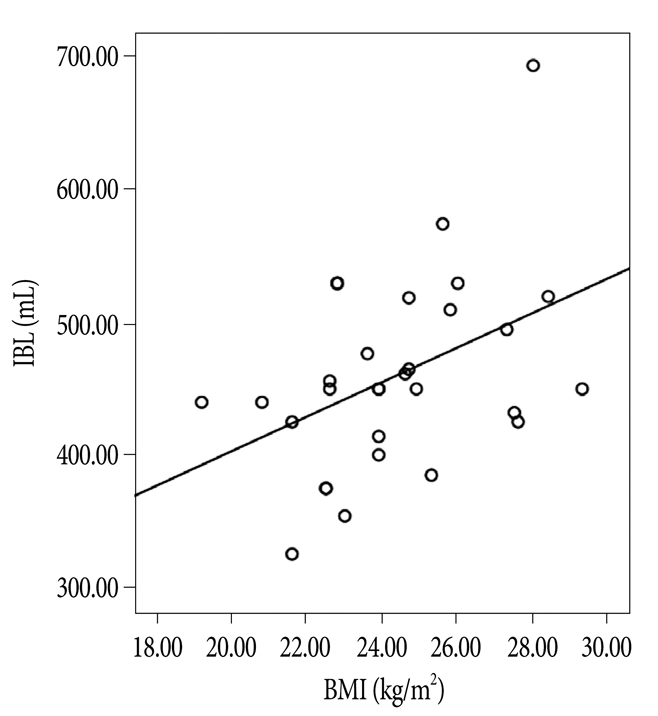
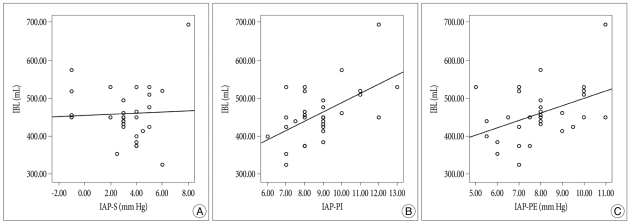
IAP in the supine position was not significantly different in groups 1, 2, and 3 (2.7 mm Hg, 3.0 mm Hg, and 4.2 mm Hg, respectively) (p=0.258), and IAP in the prone position at incision increased to 7.8 mm Hg, 8.2 mm Hg, and 10.4 mm Hg, respectively, in the three groups, and these intergroup differences were significant, especially for Group 3 (p=0.000). IAP at the end of surgery was slightly lower (7.0 mm Hg, 7.7 mm Hg, and 9.2 mm Hg, respectively). IBLs were not significantly different between the three groups. However, IBLs were found to increase with IAP in the prone position (p=0.022) and BMI (p<0.05).
CONCLUSION
These results show that BMI affects IAP in the prone position more than in the supine position during lumbar spinal surgery. In addition, IBLs were found to increase with IAP in the prone position and with BMI. Thus, IBLs can be expected to be higher in morbidly obese patients due to an increased IAP.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Cushing Syndrome: A Potential Risk of Bilateral Postoperative Ischemic Optic Neuropathy after Lumbar Fusion
Bumsoo Park, Seung-Won Choi, Sanghyun Han, Jin-Young Youm, Jeong-Wook Lim, Hyon-Jo Kwon
Korean J Neurotrauma. 2019;15(2):221-226. doi: 10.13004/kjnt.2019.15.e39.
Reference
-
1. Aono H, Ohwada T, Hosono N, Tobimatsu H, Ariga K, Fuji T, et al. Incidence of postoperative symptomatic epidural hematoma in spinal decompression surgery. J Neurosurg Spine. 2011; 15:202–205. PMID: 21529204.
Article2. Batson OV. The function of the vertebral veins and their role in the spread of metastases. 1940. Clin Orthop Relat Res. 1995; 4–9. PMID: 7634616.3. Böstman O, Hyrkäs J, Hirvensalo E, Kallio E. Blood loss, operating time, and positioning of the patient in lumbar disc surgery. Spine (Phila Pa 1976). 1990; 15:360–363. PMID: 2363066.
Article4. Cobb WS, Burns JM, Kercher KW, Matthews BD, James Norton H, Todd Heniford B. Normal intraabdominal pressure in healthy adults. J Surg Res. 2005; 129:231–235. PMID: 16140336.
Article5. Fusco MA, Martin RS, Chang MC. Estimation of intra-abdominal pressure by bladder pressure measurement : validity and methodology. J Trauma. 2001; 50:297–302. PMID: 11242295.
Article6. Imagama S, Kawakami N, Tsuji T, Ohara T, Matsubara Y, Kanemura T, et al. Perioperative complications and adverse events after lumbar spinal surgery : evaluation of 1012 operations at a single center. J Orthop Sci. 2011; 16:510–515. PMID: 21725670.
Article7. Karikari IO, Isaacs RE. Minimally invasive transforaminal lumbar interbody fusion : a review of techniques and outcomes. Spine (Phila Pa 1976). 2010; 35:S294–S301. PMID: 21160393.8. Kou J, Fischgrund J, Biddinger A, Herkowitz H. Risk factors for spinal epidural hematoma after spinal surgery. Spine (Phila Pa 1976). 2002; 27:1670–1673. PMID: 12163731.
Article9. Kron IL, Harman PK, Nolan SP. The measurement of intra-abdominal pressure as a criterion for abdominal re-exploration. Ann Surg. 1984; 199:28–30. PMID: 6691728.
Article10. Lin PM. A technical modification of Cloward's posterior lumbar interbody fusion. Neurosurgery. 1977; 1:118–124. PMID: 355915.
Article11. Park CK. The effect of patient positioning on intraabdominal pressure and blood loss in spinal surgery. Anesth Analg. 2000; 91:552–557. PMID: 10960374.
Article12. Rigamonti A, Gemma M, Rocca A, Messina M, Bignami E, Beretta L. Prone versus knee-chest position for microdiscectomy : a prospective randomized study of intra-abdominal pressure and intraoperative bleeding. Spine (Phila Pa 1976). 2005; 30:1918–1923. PMID: 16135980.
Article13. Sanchez NC, Tenofsky PL, Dort JM, Shen LY, Helmer SD, Smith RS. What is normal intra-abdominal pressure? Am Surg. 2001; 67:243–248. PMID: 11270882.14. Sundén G, Wallöe A, Wingstrand H. A new device to reduce intra-abdominal pressure during lumbar surgery. Spine (Phila Pa 1976). 1986; 11:635–636. PMID: 3787332.
Article15. WHO/IASO/IOTF. The Asia-Pacific perspective : redefining obesity and its treatment. 2000. Melbourne: Health Communications Australia;ISBN 0-9577082-1.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Quantifying the Amount of Bleeding and Associated Changes in Intra-Abdominal Pressure and Mean Airway Pressure in Patients Undergoing Lumbar Fixation Surgeries: A Comparison of Three Positioning Systems
- Difference of the Obesity Index, Blood Pressure and Serum Lipids in Abdominal and Non Abdominal in Men and Women
- Clinical Significance of Intra-Abdominal Hypertension
- The Influence of Central Venous Pressure on Blood Loss during Spinal Fusion in Prone Position
- The association of usual mobile telephone usage with blood pressure, body mass index, and hemoglobin