J Korean Surg Soc.
2012 Jan;82(1):8-12. 10.4174/jkss.2012.82.1.8.
Change of inter-facility transfer pattern in a regional trauma system after designation of trauma centers
- Affiliations
-
- 1Department of Emergency Medicine, Medical Research Institute, Pusan National University Hospital, Busan, Korea.
- 2Division of Trauma Surgery, Department of Surgery, Ajou University Hospital, Ajou University School of Medicine, Suwon, Korea. jake98@daum.net
- 3Department of Laboratory Medicine and Biomedical Informatics Unit, Pusan National University School of Medicine, Busan, Korea.
- 4Department of Emergency Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea.
- KMID: 1437749
- DOI: http://doi.org/10.4174/jkss.2012.82.1.8
Abstract
- PURPOSE
The Ministry of Health and Welfare recently designated 35 major trauma-specified centers (MTSC). The purpose of this study is to determine changes in patient flow and designated hospitals, and to describe the role of the emergency medical information center (EMIC) in a regional trauma care system.
METHODS
Data of trauma patient inter-facility transfer arrangement by one EMIC were reviewed for 2 months before and after the designation of MTSC. The data included success or failure rates of the arrangement, time used for arrangement, and inquiring and accepting facility.
RESULTS
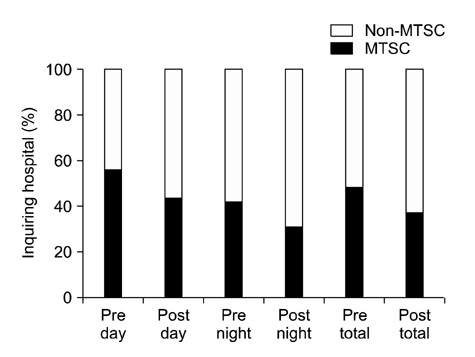
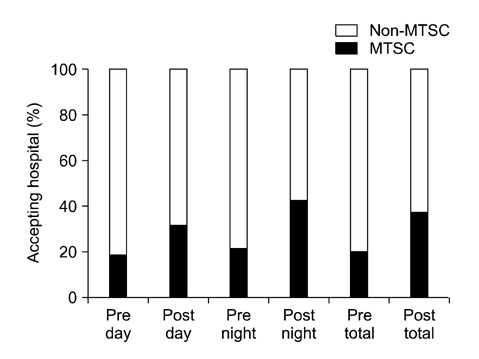
At pre- and post-designation study period, there were 540 and 433 trauma patient inter-facility transfers arranged by EMIC, respectively. The median time used for arrangement decreased from 9.3 to 7.7 minutes (P = 0.007). Arrangement failure rate was 3.5% and 2.5%, respectively, with no significant interval change (P = 0.377). The percentage of inquiring MTSC decreased from 49.1 to 36.9% (P < 0.001). The percentage of accepting MTSC increased from 20.2 to 37.4% (P < 0.001).
CONCLUSION
With the designation of MTSC, EMIC could arrange inter-facility transfers more quickly. The hospitals wanted more trauma patients after the designation. There would be a concentration of trauma patients to MTSCs in our region. Further studies are needed for scientific evidence on patient outcome.
MeSH Terms
Figure
Reference
-
1. Boyd DR, Cowley RA. Comprehensive regional trauma/emergency medical services (EMS) delivery systems: the United States experience. World J Surg. 1983. 7:149–157.2. Mann NC, Mackenzie E, Teitelbaum SD, Wright D, Anderson C. Trauma system structure and viability in the current healthcare environment: a state-by-state assessment. J Trauma. 2005. 58:136–147.3. Nathens AB, Jurkovich GJ, Rivara FP, Maier RV. Effectiveness of state trauma systems in reducing injury-related mortality: a national evaluation. J Trauma. 2000. 48:25–30.4. Guss DA, Meyer FT, Neuman TS, Baxt WG, Dunford JV Jr, Griffith LD, et al. The impact of a regionalized trauma system on trauma care in San Diego County. Ann Emerg Med. 1989. 18:1141–1145.5. West JG, Trunkey DD, Lim RC. Systems of trauma care. A study of two counties. Arch Surg. 1979. 114:455–460.6. Harrington DT, Connolly M, Biffl WL, Majercik SD, Cioffi WG. Transfer times to definitive care facilities are too long: a consequence of an immature trauma system. Ann Surg. 2005. 241:961–966.7. Glickman SW, Kit Delgado M, Hirshon JM, Hollander JE, Iwashyna TJ, Jacobs AK, et al. Defining and measuring successful emergency care networks: a research agenda. Acad Emerg Med. 2010. 17:1297–1305.8. Sasser SM, Hunt RC, Sullivent EE, Wald MM, Mitchko J, Jurkovich GJ, et al. Guidelines for field triage of injured patients. Recommendations of the National Expert Panel on Field Triage. MMWR Recomm Rep. 2009. 58(RR-1):1–35.9. Epley EE, Stewart RM, Love P, Jenkins D, Siegworth GM, Baskin TW, et al. A regional medical operations center improves disaster response and inter-hospital trauma transfers. Am J Surg. 2006. 192:853–859.10. Esposito TJ, Crandall M, Reed RL, Gamelli RL, Luchette FA. Socioeconomic factors, medicolegal issues, and trauma patient transfer trends: is there a connection? J Trauma. 2006. 61:1380–1386.11. Parks J, Gentilello LM, Shafi S. Financial triage in transfer of trauma patients: a myth or a reality? Am J Surg. 2009. 198:e35–e38.12. Position paper on trauma care systems. Third National Injury Control Conference April 22-25, 1991, Denver, Colorado. J Trauma. 1992. 32:127–129.13. Model trauma system planning and evaluation. US Department of Health and Human Services, Health Resources and Services Administration. 2006. cited 2011 July 1. Washington DC: US Department of Health and Human Services;Available from: http://www.kstrauma.org/download/ModelTraumaSystemPlanningandEvaluation.pdf.14. Trauma system maturity index [Internet]. World Health Organization. c2011. cited 2011 July 1. Geneva: WHO;Available from: http://www.who.int/violence_injury_prevention/services/traumacare/maturity_index/en/index.html.15. Ting HH, Rihal CS, Gersh BJ, Haro LH, Bjerke CM, Lennon RJ, et al. Regional systems of care to optimize timeliness of reperfusion therapy for ST-elevation myocardial infarction: the Mayo Clinic STEMI Protocol. Circulation. 2007. 116:729–736.16. Henry TD, Unger BT, Sharkey SW, Lips DL, Pedersen WR, Madison JD, et al. Design of a standardized system for transfer of patients with ST-elevation myocardial infarction for percutaneous coronary intervention. Am Heart J. 2005. 150:373–384.17. Kim SK, Lee SY, Bae HJ, Lee YS, Kim SY, Kang MJ, et al. Pre-hospital notification reduced the door-to-needle time for iv t-PA in acute ischaemic stroke. Eur J Neurol. 2009. 16:1331–1335.18. Lossius HM, Kristiansen T, Ringdal KG, Rehn M. Interhospital transfer: the crux of the trauma system, a curse for trauma registries. Scand J Trauma Resusc Emerg Med. 2010. 18:15.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Background and progress of regional trauma center development
- Understanding Regional Trauma Centers and managing a trauma care system in South Korea: a systematic review
- Proposal for stabilization of regional trauma centers in Korea
- A Review of Quality Management and Improvement of Trauma Fee Schedule in Regional Trauma Center
- Impact of trauma center care on mortality in Gangwon Province in Korea