J Korean Assoc Oral Maxillofac Surg.
2012 Feb;38(1):38-43. 10.5125/jkaoms.2012.38.1.38.
Preoperative prediction of the location of parotid gland tumors using radiographic anatomical landmarks
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Kyungpook National University School of Dentistry, Daegu, Korea. vocaleo@knu.ac.kr
- 2Department of Oral and Maxillofacial Radiology, Kyungpook National University School of Dentistry, Daegu, Korea.
- KMID: 1434377
- DOI: http://doi.org/10.5125/jkaoms.2012.38.1.38
Abstract
- INTRODUCTION
The location of parotid gland tumors in the superficial or deep lobes can affect the time and difficulty of operations. Therefore, accurate preoperative evaluation of the tumor location is important for surgical outcomes.
MATERIALS AND METHODS
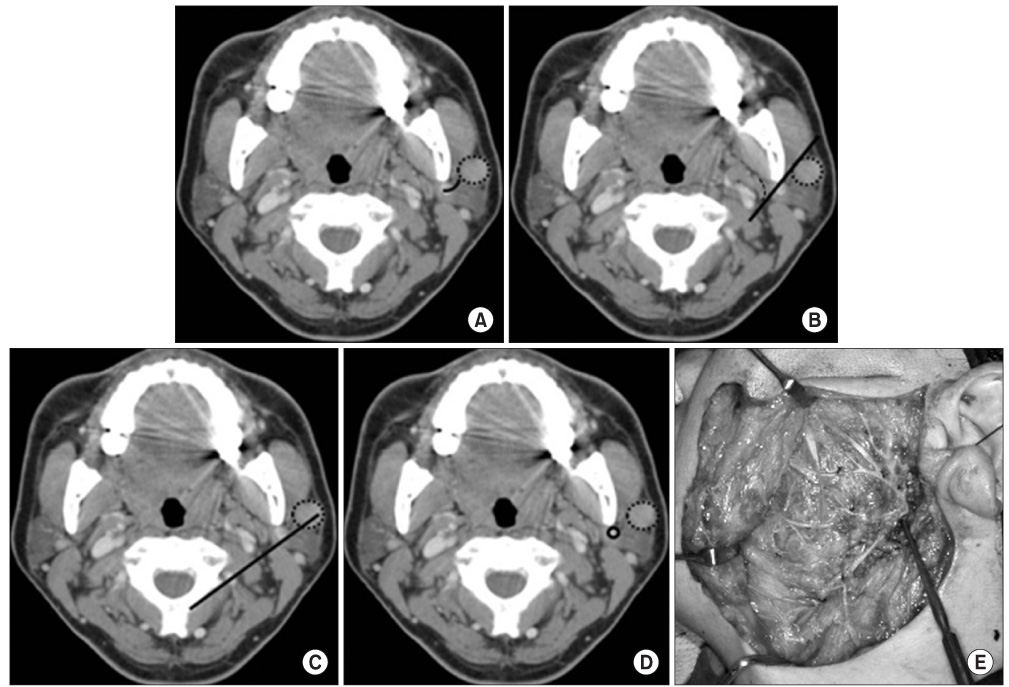
A total of 16 patients with parotid gland tumors and who underwent a parotidectomy between April 2003 and March 2011 were retrospectively reviewed in terms of demographic background, tumor location, surgical treatment, and treatment outcomes. Tumor location was estimated by four landmarks on contrast enhanced computerized tomography scans, which were Conn's arc, the facial nerve (FN) line, the Utrecht line, and the retromandibular vein. Tumor location was confirmed by relative position depending on the facial nerve during surgery. It was assumed positive since the tumor lies in the superficial lobe of the parotid gland, the sensitivity, specificity, positive predictive value, negative predictive value, and efficiency of each landmark were evaluated.
RESULTS
Our result revealed that the facial nerve line had a sensitivity of 83.3%, specificity of 100%, positive predictive value of 100%, negative predictive value of 71.4%, and efficiency of 87.5%. Some would be more efficient preoperative evaluation methods of the relationship of parotid gland tumors to the facial nerve than others.
CONCLUSION
In our study, the FN line was found to be the most reliable analysis method.
MeSH Terms
Figure
Reference
-
1. Lim CY, Chang HS, Nam KH, Chung WY, Park CS. Preoperative prediction of the location of parotid gland tumors using anatomical landmarks. World J Surg. 2008. 32:2200–2203.
Article2. de Ru JA, van Benthem PP, Hordijk GJ. The location of parotid gland tumors in relation to the facial nerve on magnetic resonance images and computed tomography scans. J Oral Maxillofac Surg. 2002. 60:992–994.
Article3. DelBalso AM, Ellis GE, Hartman KS, Langlais RP. Del Balso AM, editor. Diagnostic imaging of the salivary glands and periglandular regions. Maxillofacial imaging. 1990. Philadelphia: WB Saunders;87–93.4. Smith JR, King WW, Tang WY, Metreweli C. Differentiating tumours of the deep and superficial lobes of the parotid gland by computed tomographic sialography. Clin Radiol. 1987. 38:345–349.
Article5. Stone DN, Mancuso AA, Rice D, Hanafee WN. Parotid CT sialography. Radiology. 1981. 138:393–397.
Article6. Rice DH, Mancuso AA, Hanafee WN. Computerized tomography with simultaneous sialography in evaluating parotid tumors. Arch Otolaryngol. 1980. 106:472–473.
Article7. Sone S, Higashihara T, Morimoto S, Ikezoe J, Nakatsukasa M, Arisawa J, et al. CT of parotid tumors. AJNR Am J Neuroradiol. 1982. 3:143–147.8. Wittich GR, Scheible WF, Hajek PC. Ultrasonography of the salivary glands. Radiol Clin North Am. 1985. 23:29–37.9. de Ru JA, Bleys RL, van Benthem PP, Hordijk GJ. Preoperative determination of the location of parotid gland tumors by analysis of the position of the facial nerve. J Oral Maxillofac Surg. 2001. 59:525–528.
Article10. Conn IG, Wiesenfeld D, Ferguson MM. The anatomy of the facial nerve in relation to CT/sialography of the parotid gland. Br J Radiol. 1983. 56:901–905.
Article11. Ariyoshi Y, Shimahara M. Determining whether a parotid tumor is in the superficial or deep lobe using magnetic resonance imaging. J Oral Maxillofac Surg. 1998. 56:23–26.
Article12. Kurabayashi T, Ida M, Ohbayashi N, Ishii J, Sasaki T. Criteria for differentiating superficial from deep lobe tumours of the parotid gland by computed tomography. Dentomaxillofac Radiol. 1993. 22:81–85.
Article13. Thibault F, Halimi P, Bely N, Chevallier JM, Bonfils P, Lellouch-Tubiana A, et al. Internal architecture of the parotid gland at MR imaging: facial nerve or ductal system? Radiology. 1993. 188:701–704.
Article14. Teresi LM, Lufkin RB, Wortham DG, Abemayor E, Hanafee WN. Parotid masses: MR imaging. Radiology. 1987. 163:405–409.
Article15. Tabor EK, Curtin HD. MR of the salivary glands. Radiol Clin North Am. 1989. 27:379–392.16. Ragbir M, Dunaway DJ, Chippindale AJ, Latimer J, Mohammed F, McLean NR. Prediction of the position of the intraparotid portion of the facial nerve on MRI and CT. Br J Plast Surg. 2002. 55:376–379.
Article17. Agur AMR, Lee MJ. Grant's atlass of anatomy. 1999. 10th ed. Philadelphia: Lippincott W&W.18. Charles WC, John MF, Lee AH, Carles JK, David ES. Otolaryngology-head and neck surgery. 1986. St. Louis: C.V Mosby.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prediction of Location of the Parotid Tumors that Cross Over Anatomical Criteria for Facial Nerve on Computed Tomography
- Clinical Study of Parotid Gland Tumors
- Anatomical Variation of Facial Nerve during Parotid Surgery
- Surgical Treatment of Primary and Metastatic Malignant Tumors of the Accessory Parotid Gland
- 6 Cases of Salivary Gland Tumors Arising at Buccal and Masseteric Area