J Korean Assoc Oral Maxillofac Surg.
2012 Oct;38(5):305-309. 10.5125/jkaoms.2012.38.5.305.
Chronic dislocation of temporomandibular joint persisting for 6 months: a case report
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, College of Dentistry, Dankook University, Cheonan, Korea. kimchoms@dankook.ac.kr
- KMID: 1434333
- DOI: http://doi.org/10.5125/jkaoms.2012.38.5.305
Abstract
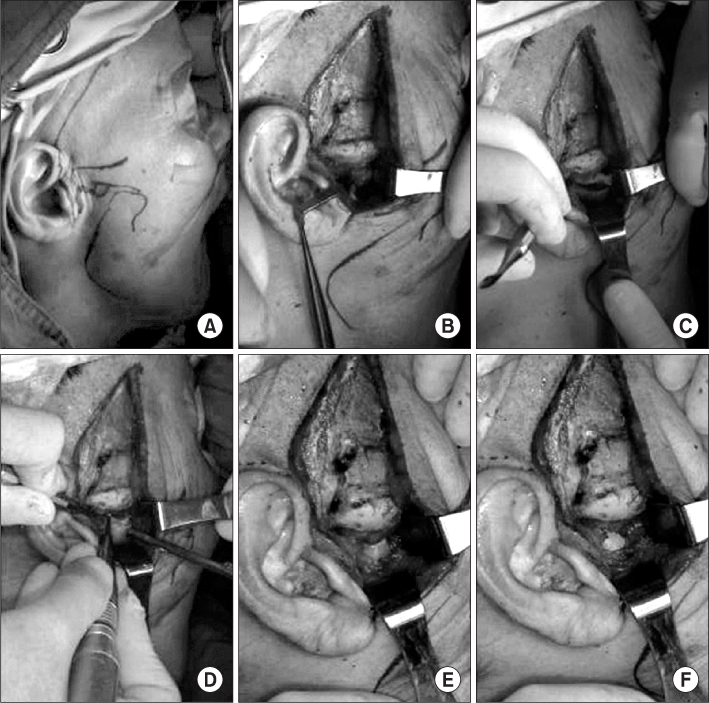
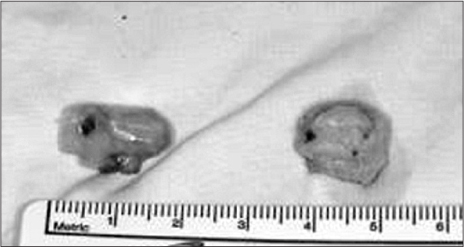
- Temporomandibular joint (TMJ) subluxation and dislocation are uncommon but very unpleasant and distressing conditions to patients. Subluxation of the TMJ is an excessively abnormal condylar excursion secondary to flaccidity and laxity of the capsule. When the condyle head excurses anterior to the eminence upon wide opening, it can return to the fossa by self-manipulation or non-surgical conservative reduction. Surgery is recommended if a complete dislocation, so-called open lock, occurs as a chronic or recurrent protracted condition that cannot be reduced voluntarily. A range of surgical procedures can be performed to limit condylar hypermobility inclusing soft tissue tethering, creation of articular obstacles, removal of mechanical blockade and augmentation of articular eminence using different kinds of grafts. In the present case, a 74-year-old woman was diagnosed with a chronic TMJ dislocation that had lasted for 6 months. Bilateral condylectomy was performed and the post-operative results were good without functional limitations or recurrence.
Keyword
Figure
Reference
-
1. Kim CH, Kim H. Surgical correction of recurrent habitual temporomandibular joint dislocation. J Korean Assoc Oral Maxillofac Surg. 1998. 24:365–369.2. Merrill RG. Habitual subluxation and recurrent dislocation in a patient with Parkinson's disease: report of case. J Oral Surg. 1968. 26:473–477.3. Irby WB. Surgical correction of chronic dislocation of the temporomandibular joint not responsive to conservative therapy. J Oral Surg (Chic). 1957. 15:307–312.4. Myrhaug H. A new method of operation for habitual dislocation of the mandible; review of former methods of treatment. Acta Odontol Scand. 1951. 9:247–260.5. Georgiade N. The surgical correction of chronic luxation of the mandibular condyle. Plast Reconstr Surg. 1965. 36:339–342.
Article6. Merrill RG. Keith DA, editor. Mandibular dislocation. Surgery of the temporomandibular joint. 1988. London: Blackwell Publications;135–168.7. Lawlor MG. Recurrent dislocation of the mandible: treatment of ten cases by the Dautrey procedure. Br J Oral Surg. 1982. 20:14–21.
Article8. Puelacher WC, Waldhart E. Miniplate eminoplasty: a new surgical treatment for TMJ-dislocation. J Craniomaxillofac Surg. 1993. 21:176–178.
Article9. Howe AG, Kent JN, Farrell CD, Poidmore SJ. Implant of articular eminence for recurrent dislocation of the temporomandibular joint. J Oral Surg. 1978. 36:523–526.10. Whear NM, Langdon JD, Macpherson DW. Temporomandibular joint eminence augmentation by down-fracture and inter-positional cartilage graft. A new surgical technique. Int J Oral Maxillofac Surg. 1991. 20:357–359.
Article11. Mangi Q, Ridgway PF, Ibrahim Z, Evoy D. Dislocation of the mandible. Surg Endosc. 2004. 18:554–556.
Article12. Ziegler CM, Haag C, Muhling J. Treatment of recurrent temporomandibular joint dislocation with intramuscular botulinum toxin injection. Clin Oral Investig. 2003. 7:52–55.
Article13. Kato T, Shimoyama T, Nasu D, Kaneko T, Horie N, Kudo I. Autologous blood injection into the articular cavity for the treatment of recurrent temporomandibular joint dislocation: a case report. J Oral Sci. 2007. 49:237–239.
Article14. O'hara VS. Extrapyramidal reactions in patients receiving prochlorperazine. N Engl J Med. 1958. 259:826–828.15. Beighton P, Horan F. Orthopaedic aspects of the Ehlers-Danlos syndrome. J Bone Joint Surg Br. 1969. 51:444–453.16. Kojetzny GE. Die Behandlung der habituellen Luxation der sogenannten habituellen subluxation des Underkiefers u d Kiefergelenksknachens. Z Chir. 1929. 56:3018.17. Pogrel MA, Kaban LB. The role of a temporalis fascia and muscle flap in temporomandibular joint surgery. J Oral Maxillofac Surg. 1990. 48:14–19.
Article18. LeClere GC, Girard C. Un nouveau procede de butee dans le traitement chirurgical de la luxation recidivante de la machoire inferieure. Mem Acad Chir. 1943. 69:451.19. Kaban LB, Perrott DH, Fisher K. A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 1990. 48:1145–1151.
Article20. Sato J, Segami N, Nishimura M, Suzuki T, Kaneyama K, Fujimura K. Clinical evaluation of arthroscopic eminoplasty for habitual dislocation of the temporomandibular joint: comparative study with conventional open eminectomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003. 95:390–395.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unrecognized Bilateral Dislocation of Temporomandibular Joint during Orotracheal Intubation
- Dislocation of the Bilateral Temporomandibular Joint due to Generalized Tonic-Clonic Seizures
- SURGICAL CORRECTION OF RECURRENT HABITUAL TEMPOROMANDIBULAR JOINT DISLOCATION
- Open Lock of the Jaw on Induction of Anesthesia: A case report
- Condylar Hyperplasia with Long-standing Temporomandibular Joint Dislocation