J Korean Surg Soc.
2013 Sep;85(3):139-144. 10.4174/jkss.2013.85.3.139.
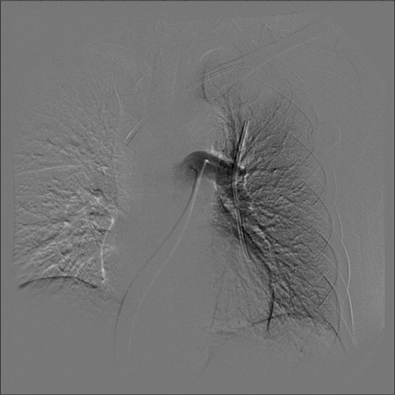
Pinch-off syndrome
- Affiliations
-
- 1Department of Surgery, Bucheon St. Mary's Hospital, The Catholic University of Korea College of Medicine, Bucheon, Korea. dosangs@catholic.ac.kr
- KMID: 1426347
- DOI: http://doi.org/10.4174/jkss.2013.85.3.139
Abstract
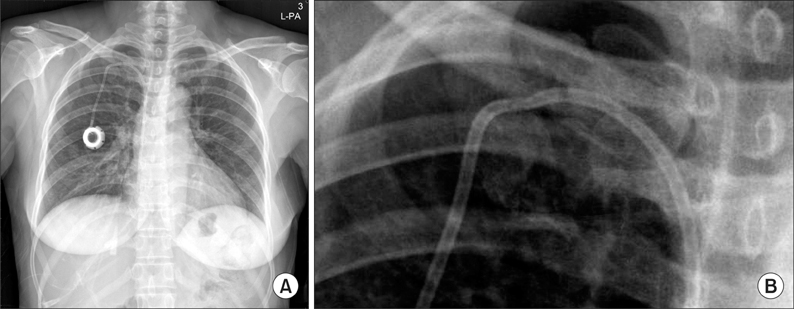
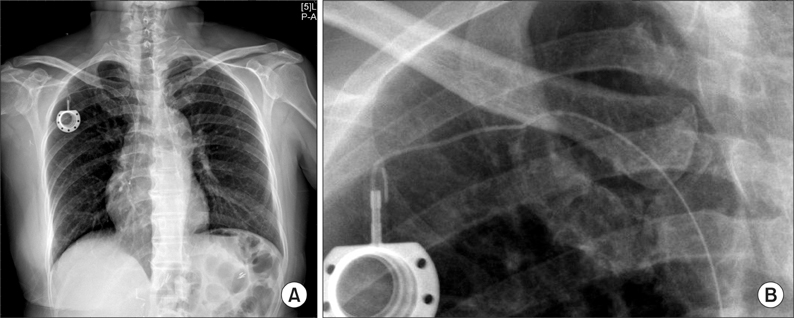
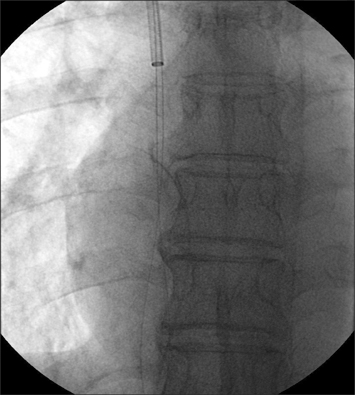
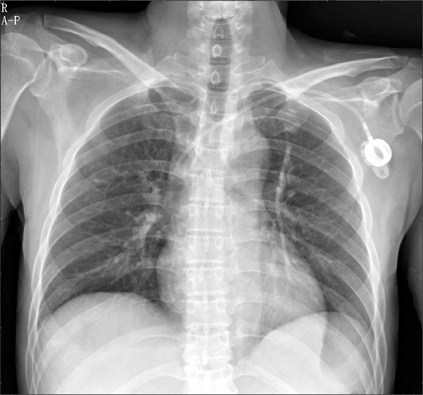
- Subclavian venous catheterization was previously frequently performed, but because of life-threatening complications such as hemothorax, pneumothorax, mediastinal hematoma, and myocardial injury, its use has become less common. However, this practice has some advantages in patient mobility, secured dressing, and rapidity and adequacy of vascular access. In some situations where patient comfort is an especially important consideration, such as with totally implantable venous port insertion for chemotherapy, the subclavian route can be a good choice if an experienced and well-trained faculty is available. The authors have had recent experience with pinch-off syndrome-in other words, spontaneous catheter fracture-in 3 patients who had undergone venous port implantation through the right subclavian route. Through these cases, we intend to review the dangers of subclavian venous catheterization, the causes of pinch-off syndrome, and its clinical presentation, progress, treatments, and prevention.
Keyword
Figure
Cited by 1 articles
-
Catheter Fracture of a Totally Implantable Venous Device Due to Pinch Off Syndrome in Breast Cancer: A Case Report
Yoonseok Kim
Kosin Med J. 2016;31(2):167-172. doi: 10.7180/kmj.2016.31.2.167.
Reference
-
1. Slama M, Novara A, Safavian A, Ossart M, Safar M, Fagon JY. Improvement of internal jugular vein cannulation using an ultrasound-guided technique. Intensive Care Med. 1997; 23:916–919.2. Karakitsos D, Labropoulos N, De Groot E, Patrianakos AP, Kouraklis G, Poularas J, et al. Real-time ultrasound-guided catheterisation of the internal jugular vein: a prospective comparison with the landmark technique in critical care patients. Crit Care. 2006; 10:R162.3. Hinke DH, Zandt-Stastny DA, Goodman LR, Quebbeman EJ, Krzywda EA, Andris DA. Pinch-off syndrome: a complication of implantable subclavian venous access devices. Radiology. 1990; 177:353–356.4. Aitken DR, Minton JP. The "pinch-off sign": a warning of impending problems with permanent subclavian catheters. Am J Surg. 1984; 148:633–636.5. Mirza B, Vanek VW, Kupensky DT. Pinch-off syndrome: case report and collective review of the literature. Am Surg. 2004; 70:635–644.6. Fisher RG, Ferreyro R. Evaluation of current techniques for nonsurgical removal of intravascular iatrogenic foreign bodies. AJR Am J Roentgenol. 1978; 130:541–548.7. De Moor B, Vanholder R, Ringoir S. Subclavian vein hemodialysis catheters: advantages and disadvantages. Artif Organs. 1994; 18:293–297.8. Rubenstein RB, Alberty RE, Michels LG, Pederson RW, Rosenthal D. Hickman catheter separation. JPEN J Parenter Enteral Nutr. 1985; 9:754–757.9. Zieren J, Thul P, Romaniuk P, Muller JM. Intravascular disruption of central venous ports. Clin Nutr. 1998; 17:89–91.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reliability of the Pinch Strength with Digitalized Pinch Dynamometer
- The Study of Pinching Type and Power
- Catheter Fracture of a Totally Implantable Venous Device Due to Pinch Off Syndrome in Breast Cancer: A Case Report
- Analysis of Grip and Pinch Strength in Korean People
- Changes in the Hand Strength and Related Factors after Carpal Tunnel Decompression