Predictors and Clinical Impact of Inappropriate Implantable Cardioverter-Defibrillator Shocks in Korean Patients
- Affiliations
-
- 1Division of Cardiology, Department of Medicine, Cardiac and Vascular Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. yk.on@samsung.com
- 2Department of Pediatrics, Cardiac and Vascular Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1421613
- DOI: http://doi.org/10.3346/jkms.2012.27.6.619
Abstract
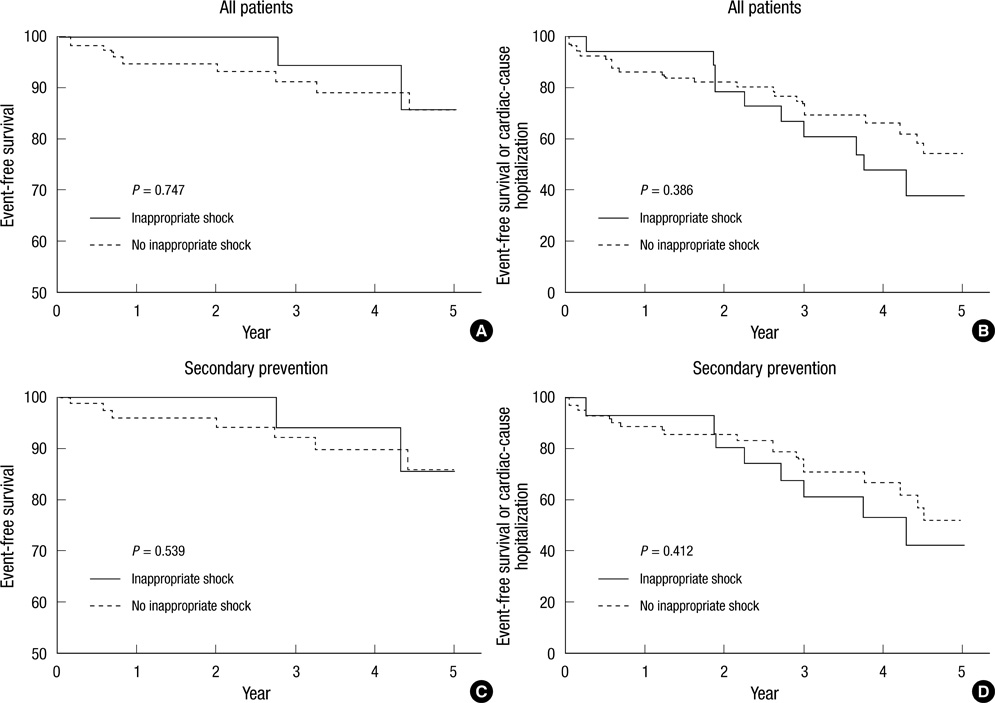
- Limited data are available on inappropriate shocks in Korean patients implanted with an implantable cardioverter-defibrillator (ICD). We investigated the impact of inappropriate shocks on clinical outcomes. This retrospective, single-center study included 148 patients treated between October 1999 and June 2011. The primary outcome was a composite event of all-cause mortality or hospitalization for any cardiac reason. The median follow-up duration was 29 months (interquartile range: 8 to 53). One or more inappropriate shocks occurred in 34 (23.0%) patients. A history of atrial fibrillation was the only independent predictor of inappropriate shock (hazard ratio [HR]: 4.16, 95% confidence interval [CI]: 1.89-9.15, P < 0.001). Atrial fibrillation was the most common cause of inappropriate shock (67.7%), followed by supraventricular tachycardia (23.5%), and abnormal sensing (8.8%). A composite event of all-cause mortality or hospitalizations for any cardiac reason during follow-up was not significantly different between patients with or without inappropriate shock (inappropriate shock vs no inappropriate shock: 35.3% vs 35.4%, adjusted HR: 1.06, 95% CI: 0.49-2.29, P = 0.877). Inappropriate shocks do not affect clinical outcomes in patients implanted with an ICD, although the incidence of inappropriate shocks is high.
MeSH Terms
-
Adult
Aged
Atrial Fibrillation/complications
Defibrillators, Implantable/*adverse effects
Equipment Failure
Female
Hospitalization
Humans
Kaplan-Meier Estimate
Male
Middle Aged
*Predictive Value of Tests
Republic of Korea
Retrospective Studies
Risk Factors
Shock/*etiology/mortality
Tachycardia, Supraventricular/complications
Figure
Cited by 3 articles
-
Implantable Cardioverter-defibrillator Utilization and Its Outcomes in Korea: Data from Korean Acute Heart Failure Registry
Youngjin Cho, Sang-Yeong Cho, Il-Young Oh, Ji Hyun Lee, Jin Joo Park, Hae-Young Lee, Kye Hun Kim, Byung-Su Yoo, Seok-Min Kang, Sang Hong Baek, Eun-Seok Jeon, Jae-Joong Kim, Myeong-Chan Cho, Shung Chull Chae, Byung-Hee Oh, Dong-Ju Choi
J Korean Med Sci. 2020;35(46):e397. doi: 10.3346/jkms.2020.35.e397.Long-Term Prognosis of Patients with an Implantable Cardioverter-Defibrillator in Korea
Jae-Sun Uhm, Tae-Hoon Kim, In-Cheol Kim, Young-Ah Park, Dong Geum Shin, Yeong-Min Lim, Hee-Tae Yu, Pil-Sung Yang, Hui-Nam Pak, Seok-Min Kang, Moon-Hyoung Lee, Boyoung Joung
Yonsei Med J. 2017;58(3):514-520. doi: 10.3349/ymj.2017.58.3.514.Clinical Impact of Implantable Cardioverter-Defibrillator Therapy and Mortality Prediction Model for Effective Primary Prevention in Korean Patients
Myung Hwan Bae, Yongkeun Cho, Jongmin Hwang, Hyoung-Seob Park, Seongwook Han, Young Soo Lee, Hyun Jun Cho, Byung Chun Jung, Chan-Hee Lee, Dae-Woo Hyun, Jong Sung Park, Jinhee Ahn, Ki-Hun Kim, Dong-Gu Shin
J Korean Med Sci. 2020;35(9):. doi: 10.3346/jkms.2020.35.e49.
Reference
-
1. Moss AJ, Hall WJ, Cannom DS, Daubert JP, Higgins SL, Klein H, Levine JH, Saksena S, Waldo AL, Wilber D, et al. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. N Engl J Med. 1996. 335:1933–1940.2. Kadish A, Dyer A, Daubert JP, Quigg R, Estes NA, Anderson KP, Calkins H, Hoch D, Goldberger J, Shalaby A, et al. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med. 2004. 350:2151–2158.3. Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005. 352:225–237.4. Kim YH, Kim JS. Clinical characteristics in patients with implantable cardioverter-defibrillator (ICD). Korean Circ J. 2004. 34:395–404.5. Song PS, Kim JS, Shin DH, Park JW, Bae KI, Lee CH, Jung DC, Ryu DR, On YK. Electrical storms in patients with an implantable cardioverter defibrillator. Yonsei Med J. 2011. 52:26–32.6. Schron EB, Exner DV, Yao Q, Jenkins LS, Steinberg JS, Cook JR, Kutalek SP, Friedman PL, Bubien RS, Page RL, et al. Quality of life in the antiarrhythmics versus implantable defibrillators trial: impact of therapy and influence of adverse symptoms and defibrillator shocks. Circulation. 2002. 105:589–594.7. Lüderitz B, Jung W, Deister A, Marneros A, Manz M. Patient acceptance of the implantable cardioverter defibrillator in ventricular tachyarrhythmias. Pacing Clin Electrophysiol. 1993. 16:1815–1821.8. Dichtl W, Wolber T, Paoli U, Brüllmann S, Stühlinger M, Berger T, Spuller K, Strasak A, Pachinger O, Haegeli LM, et al. Appropriate therapy but not inappropriate shocks predict survival in implantable cardioverter defibrillator patients. Clin Cardiol. 2011. 34:433–436.9. Cevik C, Perez-Verdia A, Nugent K. Implantable cardioverter defibrillators and their role in heart failure progression. Europace. 2009. 11:710–715.10. Higgins SL, Lee RS, Kramer RL. Stability: an ICD detection criterion for discriminating atrial fibrillation from ventricular tachycardia. J Cardiovasc Electrophysiol. 1995. 6:1081–1088.11. Kühlkamp V, Dörnberger V, Mewis C, Suchalla R, Bosch RF, Seipel L. Clinical experience with the new detection algorithms for atrial fibrillation of a defibrillator with dual chamber sensing and pacing. J Cardiovasc Electrophysiol. 1999. 10:905–915.12. van Rees JB, Borleffs CJ, de Bie MK, Stijnen T, van Erven L, Bax JJ, Schalij MJ. Inappropriate implantable cardioverter-defibrillator shocks: incidence, predictors, and impact on mortality. J Am Coll Cardiol. 2011. 57:556–562.13. Daubert JP, Zareba W, Cannom DS, McNitt S, Rosero SZ, Wang P, Schuger C, Steinberg JS, Higgins SL, Wilber DJ, et al. Inappropriate implantable cardioverter-defibrillator shocks in MADIT II: frequency, mechanisms, predictors, and survival impact. J Am Coll Cardiol. 2008. 51:1357–1365.14. Germano JJ, Reynolds M, Essebag V, Josephson ME. Frequency and causes of implantable cardioverter-defibrillator therapies: is device therapy proarrhythmic? Am J Cardiol. 2006. 97:1255–1261.15. Bhavnani SP, Coleman CI, White CM, Clyne CA, Yarlagadda R, Guertin D, Kluger J. Association between statin therapy and reductions in atrial fibrillation or flutter and inappropriate shock therapy. Europace. 2008. 10:854–859.16. Kleemann T, Becker T, Doenges K, Vater M, Senges J, Schneider S, Saggau W, Weisse U, Seidl K. Annual rate of transvenous defibrillation lead defects in implantable cardioverter-defibrillators over a period of >10 years. Circulation. 2007. 115:2474–2480.17. Keren A, Sears SF, Nery P, Shaw J, Green MS, Lemery R, Gollob MH, Amyotte B, Birnie DH. Psychological adjustment in ICD patients living with advisory fidelis leads. J Cardiovasc Electrophysiol. 2011. 22:57–63.18. Marcus GM, Chan DW, Redberg RF. Recollection of pain due to inappropriate versus appropriate implantable cardioverter-defibrillator shocks. Pacing Clin Electrophysiol. 2011. 34:348–353.19. Lo R, Al-Ahmad A, Hsia H, Zei PC, Wang PJ. Optimal Programming of ICDs for Prevention of Appropriate and Inappropriate Shocks. Curr Treat Options Cardiovasc Med. 2008. 10:408–416.20. Swerdlow CD, Gunderson BD, Ousdigian KT, Abeyratne A, Sachanandani H, Ellenbogen KA. Downloadable software algorithm reduces inappropriate shocks caused by implantable cardioverter-defibrillator lead fractures: a prospective study. Circulation. 2010. 122:1449–1455.21. Auricchio A, Meijer A, Kurita T, Schloss E, Brinkman K, Claessens-van Ooijen M, Sterns L. Safety, efficacy, and performance of new discrimination algorithms to reduce inappropriate and unnecessary shocks: the PainFree SST clinical study design. Europace. 2011. 13:1484–1493.22. Gold MR, Ahmad S, Browne K, Berg KC, Thackeray L, Berger RD. Prospective comparison of discrimination algorithms to prevent inappropriate ICD therapy: primary results of the Rhythm ID Going Head to Head Trial. Heart Rhythm. 2012. 9:370–377.23. Moss AJ, Greenberg H, Case RB, Zareba W, Hall WJ, Brown MW, Daubert JP, McNitt S, Andrews ML, Elkin AD. Long-term clinical course of patients after termination of ventricular tachyarrhythmia by an implanted defibrillator. Circulation. 2004. 110:3760–3765.24. Poole JE, Johnson GW, Hellkamp AS, Anderson J, Callans DJ, Raitt MH, Reddy RK, Marchlinski FE, Yee R, Guarnieri T, et al. Prognostic importance of defibrillator shocks in patients with heart failure. N Engl J Med. 2008. 359:1009–1017.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Short-Long R-R Sequence Induced Implantable Cardioverter Defibrillator Shock by Dislodged Lead Even Having Normal Interrogation Parameter
- Where is the Lead? Inappropriate Implantable Cardioverter-Defibrillator Shock Caused by Extreme Twiddling
- Transvenous Implantation of an Implantable Cardioverter Defibrillator in a Patient Who Had Undergone Tricuspid Valve Replacement
- A Case Report of the Patient Implanted with Automatic Implantable Cardioverter Defibrillator (AICD) Subject to 3rd Molar Extraction using Target Controlled Infusion of Propofol and Remifentanil: A Case Report
- Tachyarrhythmia Cycle Length in Appropriate versus Inappropriate Defibrillator Shocks in Brugada Syndrome, Early Repolarization Syndrome, or Idiopathic Ventricular Fibrillation