Korean J Ophthalmol.
2012 Oct;26(5):355-361. 10.3341/kjo.2012.26.5.355.
The Clinical Features of Macular Pucker Formation after Pars Plana Vitrectomy for Primary Rhegmatogenous Retinal Detachment Repair
- Affiliations
-
- 1Department of Ophthalmology, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea. ihyun@inje.ac.kr
- 2Department of Ophthalmology, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 3Department of Ophthalmology, Gospel Hospital, Kosin University College of Medicine, Busan, Korea.
- KMID: 1397486
- DOI: http://doi.org/10.3341/kjo.2012.26.5.355
Abstract
- PURPOSE
To investigate the incidence and predisposing factors of macular pucker formation after pars plana vitrectomy in patients who developed primary rhegmatogenous retinal detachment.
METHODS
We retrospectively reviewed a consecutive series of 284 eyes in 284 patients who underwent primary retinal detachment repair by pars plana vitrectomy alone between January 1, 2009 and December 31, 2010. Patients with a history of retinal surgery or another visually significant ocular problem were excluded.
RESULTS
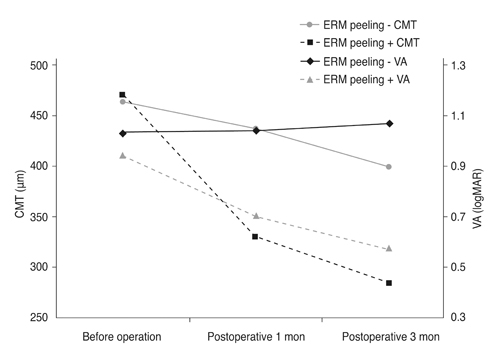
Postoperatively, of the 264 eyes that completed at least six months of follow-up, 16 (6.1%) eyes developed obvious macular pucker at clinical examination. Of these 16 eyes, ten (70.0%) underwent repeat vitrectomy with membrane peeling for macular pucker removal during the follow-up period. The mean time from primary vitrectomy for the retinal reattachment to the secondary vitrectomy with membrane peeling for macular pucker was 7.9 months. The mean improvement in vision after membrane peeling surgery was 0.37 (logarithm of the minimum angle of resolution). Using an independent t-test, chi-square test, and Mann-Whitney U-test, we found that the number or size of retinal break and vitreous hemorrhage could be significant risk factors of macular pucker.
CONCLUSIONS
In our study, 6.1% of eyes which underwent pars plana vitrectomy alone for primary retinal detachment developed a postoperative macular epiretinal membrane. Multiple or large retinal breaks and postoperative vitreous hemorrhage were related to macular pucker formation. Overall, the 70.0% of eyes which underwent secondary vitrectomy with membrane peeling for removal of macular pucker showed a favorable visual outcome.
MeSH Terms
Figure
Reference
-
1. Wilkinson CP. Visual results following scleral buckling for retinal detachments sparing the macula. Retina. 1981. 1:113–116.2. McCarty DJ, Mukesh BN, Chikani V, et al. Prevalence and associations of epiretinal membranes in the visual impairment project. Am J Ophthalmol. 2005. 140:288–294.3. Mitchell P, Smith W, Chey T, et al. Prevalence and associations of epiretinal membranes. The Blue Mountains Eye Study, Australia. Ophthalmology. 1997. 104:1033–1040.4. Avila MP, Trempe CL, Kozlowski JM, et al. Biomicroscopic study of the vitreous in eyes with macular pucker after retinal detachment surgery. Ann Ophthalmol. 1985. 17:403–410.5. Clarkson JG, Green WR, Massof D. A histopathologic review of 168 cases of preretinal membrane. Am J Ophthalmol. 1977. 84:1–17.6. Machemer R, Laqua H. Pigment epithelium proliferation in retinal detachment (massive periretinal proliferation). Am J Ophthalmol. 1975. 80:1–23.7. Machemer R, van Horn D, Aaberg TM. Pigment epithelial proliferation in human retinal detachment with massive periretinal proliferation. Am J Ophthalmol. 1978. 85:181–191.8. Michels RG. Vitrectomy for macular pucker. Ophthalmology. 1984. 91:1384–1388.9. Council MD, Shah GK, Lee HC, Sharma S. Visual outcomes and complications of epiretinal membrane removal secondary to rhegmatogenous retinal detachment. Ophthalmology. 2005. 112:1218–1221.10. Uemura A, Ideta H, Nagasaki H, et al. Macular pucker after retinal detachment surgery. Ophthalmic Surg. 1992. 23:116–119.11. Katira RC, Zamani M, Berinstein DM, Garfinkel RA. Incidence and characteristics of macular pucker formation after primary retinal detachment repair by pars plana vitrectomy alone. Retina. 2008. 28:744–748.12. Choi ES, Lee J, Oum BS, Yoon HS. The clinical feature of epiretinal membrane after retinal detachment surgery. J Korean Ophthalmol Soc. 2009. 50:1044–1049.13. Lobes LA Jr, Burton TC. The incidence of macular pucker after retinal detachment surgery. Am J Ophthalmol. 1978. 85:72–77.14. Tanenbaum HL, Schepens CL, Elzeneiny I, Freeman HM. Macular pucker following retinal detachment surgery. Arch Ophthalmol. 1970. 83:286–293.15. Cox MS, Azen SP, Barr CC, et al. Macular pucker after successful surgery for proliferative vitreoretinopathy. Silicone Study Report 8. Ophthalmology. 1995. 102:1884–1891.16. Brazitikos PD, Androudi S, Christen WG, Stangos NT. Primary pars plana vitrectomy versus scleral buckle surgery for the treatment of pseudophakic retinal detachment: a randomized clinical trial. Retina. 2005. 25:957–964.17. Schaal S, Sherman MP, Barr CC, Kaplan HJ. Primary retinal detachment repair: comparison of 1-year outcomes of four surgical techniques. Retina. 2011. 31:1500–1504.18. Massin P, Allouch C, Haouchine B, et al. Optical coherence tomography of idiopathic macular epiretinal membranes before and after surgery. Am J Ophthalmol. 2000. 130:732–739.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pars Plana Vitrectomy in Pars Planitis and Posterior Uveitis
- Pars Plana Vitrectomy in Pars Planitis and Posterior Uveitis
- A Clinical Study of Macular Pucker after Retinal Detachment Surgery
- Incidence and Risk Factors of Epiretinal Membrane Formation After Pars Plana Vitrectomy for Primary Rhegmatogenous Retinal Detachment
- The Efficacy of Pars Plana Vitrectomy on Recurrent or Remained Retinal Detachment After Primary Scleral Buckle