Korean J Radiol.
2008 Oct;9(5):458-461. 10.3348/kjr.2008.9.5.458.
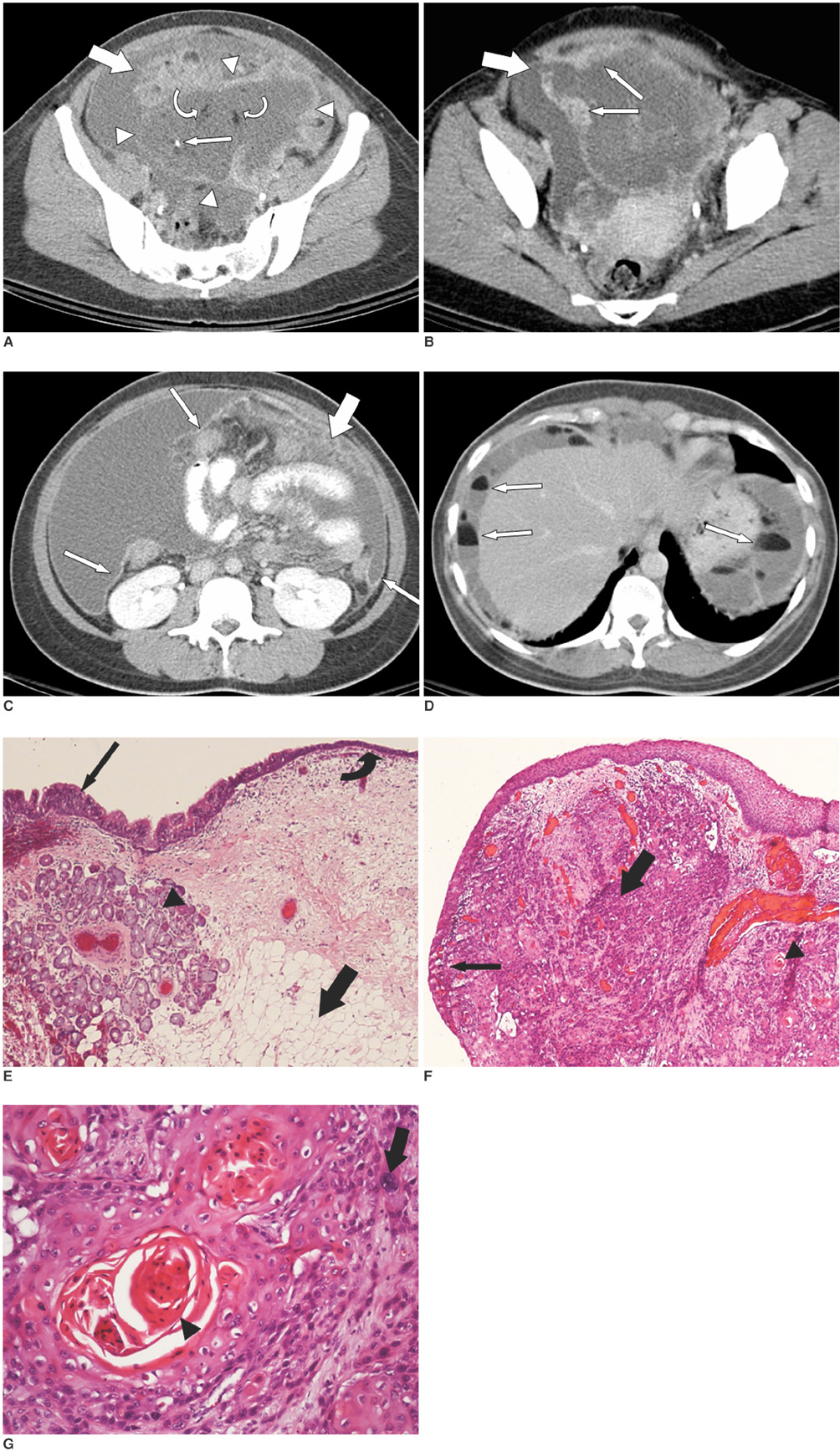
CT Images of a Malignant-Transformed Ovarian Mature Cystic Teratoma with Rupture: a Case Report
- Affiliations
-
- 1Department of Radiology, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan. tlyang.dicom@gmail.com
- 2School of Medicine, National Yang-Ming University, Taiwan.
- KMID: 1385405
- DOI: http://doi.org/10.3348/kjr.2008.9.5.458
Abstract
- A malignant transformation or a tumor rupture is a rare complication of ovarian mature cystic teratoma (MCT). A tumor rupture in a malignant-transformed MCT has never been reported in the literature. We present the CT images of a 39-year-old woman showing a large, predominantly cystic mass in the lower abdomen, with fat-fluid-level ascites. A contrast-enhanced solid component, with regional discontinuity within the cystic lesion, is also demonstrated. The pathologic diagnosis of the ruptured MCT unveils the malignant transformation (squamous cell carcinoma) and mesenteric carcinomatosis.
MeSH Terms
Figure
Reference
-
1. Rha SE, Byun JY, Jung SE, Kim HL, Oh SN, Kim H, et al. Atypical CT and MRI manifestations of mature ovarian cystic teratomas. AJR Am J Roentgenol. 2004. 183:743–750.2. Fibus TF. Intraperitoneal rupture of a benign cystic ovarian teratoma: findings at CT and MRI imaging. AJR Am J Roentgenol. 2000. 174:261–262.3. Phupong V, Sueblinvong T, Triratanachat S. Ovarian teratoma with diffused peritoneal reactions mimicking advanced ovarian malignancy. Arch Gynecol Obstet. 2004. 270:189–191.4. Levine RL, Pepe PE, Blackstone W, Danzinger J, Varon J. Occult traumatic avulsion of an ovarian dermoid cyst. Am J Emerg Med. 1992. 10:344–346.5. Abitbol MM, Pomerance W, Mackles A. Spontaneous intraperitoneal rupture of benign cystic teratomas; review of literature and report of two cases. Obstet Gynecol. 1959. 13:198–120.6. Maslin P, Luchs JS, Haas J, Katz DS. Ovarian teratoma with malignant transformation: CT diagnosis. AJR Am J Roentgenol. 2002. 178:1574.7. Lai PF, Hsieh SC, Chien JC, Fang CL, Chan WP, Yu C. Malignant transformation of an ovarian mature cystic teratoma: computed tomography findings. Arch Gynecol Obstet. 2005. 271:355–357.8. Outwater EK, Siegelman ES, Hunt JL. Ovarian teratomas: tumor types and imaging characteristics. Radiographics. 2001. 21:475–490.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Traumatic Rupture of a Mature Cystic Teratoma of the Ovary
- A Case of Adenocarcinoma Arising in Mature Cystic Teratoma of the Ovary
- Primary malignant melanoma arising from ovarian mature cystic teratoma: A case report and literature review
- Persistent chemical peritonitis resulting from spontaneous rupture of an ovarian mature cystic teratoma
- MR Findings of Malignant Struma Ovarii Associated with Mature Cystic Teratoma of Contralateral Ovary: Case Report