Clin Orthop Surg.
2012 Mar;4(1):36-44. 10.4055/cios.2012.4.1.36.
Changing Paradigms in the Treatment of Radial Club Hand: Microvascular Joint Transfer for Correction of Radial Deviation and Preservation of Long-term Growth
- Affiliations
-
- 1Division of Plastic Surgery & Department of Orthopedic Surgery, Mayo Clinic, Rochester, MN, USA. Moran.Steven@mayo.edu
- 2Departments of Hand and Microsurgery, Tampere University Hospital, Tampere, Finland.
- KMID: 1245397
- DOI: http://doi.org/10.4055/cios.2012.4.1.36
Abstract
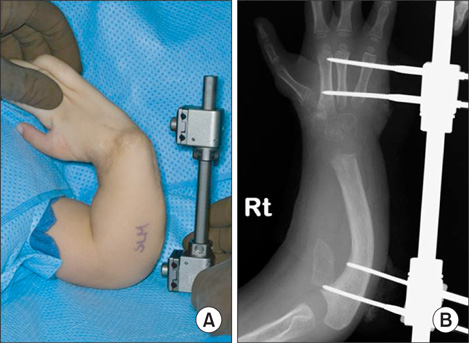
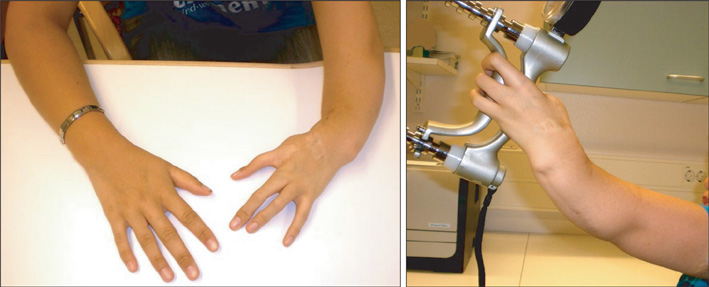
- Radial longitudinal deficiency, also known as radial club hand, is a congenital deformity of the upper extremity which can present with a spectrum of upper limb deficiencies. The typical hand and forearm deformity in such cases consists of significant forearm shortening, radial deviation of the wrist and hypoplasia or absence of a thumb. Treatment goals focus on the creation of stable centralized and functionally hand, maintenance of a mobile and stable wrist and preservation of longitudinal forearm growth. Historically centralization procedures have been the most common treatment method for this condition; unfortunately centralization procedures are associated with a high recurrence rate and have the potential for injury to the distal ulnar physis resulting in a further decrease in forearm growth. Here we advocate for the use of a vascularized second metatarsophalangeal joint transfer for stabilization of the carpus and prevention of recurrent radial deformity and subluxation of the wrist. This technique was originally described by the senior author in 1992 and he has subsequently been performed in 24 cases with an average of 11-year follow-up. In this paper we present an overview of the technique and review the expected outcomes for this method of treatment of radial longitudinal deficiency.
Keyword
MeSH Terms
Figure
Reference
-
1. James MA, Green HD, McCarroll HR Jr, Manske PR. The association of radial deficiency with thumb hypoplasia. J Bone Joint Surg Am. 2004. 86(10):2196–2205.
Article2. Maschke SD, Seitz W, Lawton J. Radial longitudinal deficiency. J Am Acad Orthop Surg. 2007. 15(1):41–52.
Article3. Ekblom AG, Laurell T, Arner M. Epidemiology of congenital upper limb anomalies in 562 children born in 1997 to 2007: a total population study from Stockholm, Sweden. J Hand Surg Am. 2010. 35(11):1742–1754.
Article4. Bayne LG, Klug MS. Long-term review of the surgical treatment of radial deficiencies. J Hand Surg Am. 1987. 12(2):169–179.
Article5. James MA, McCarroll HR Jr, Manske PR. The spectrum of radial longitudinal deficiency: a modified classification. J Hand Surg Am. 1999. 24(6):1145–1155.
Article6. Vilkki SK. Vascularized metatarsophalangeal joint transfer for radial hypoplasia. Semin Plast Surg. 2008. 22(3):195–212.
Article7. Sestero AM, Van Heest A, Agel J. Ulnar growth patterns in radial longitudinal deficiency. J Hand Surg Am. 2006. 31(6):960–967.
Article8. Shariatzadeh H, Jafari D, Taheri H, Mazhar FN. Recurrence rate after radial club hand surgery in long term follow up. J Res Med Sci. 2009. 14(3):179–186.9. Manske PR, McCarroll HR Jr, Swanson K. Centralization of the radial club hand: an ulnar surgical approach. J Hand Surg Am. 1981. 6(5):423–433.
Article10. Lamb DW. Radial club hand: a continuing study of sixty-eight patients with one hundred and seventeen club hands. J Bone Joint Surg Am. 1977. 59(1):1–13.
Article11. Sayre RH. A contribution to the study of club-hand. Trans Am Orthop Assn. 1893. 6:208–216.12. Lidge RT. Congenital radial deficient club hand. J Bone Joint Surg Am. 1969. 51(5):1041–1042.13. Watson HK, Beebe RD, Cruz NI. A centralization procedure for radial clubhand. J Hand Surg Am. 1984. 9(4):541–547.
Article14. Kessler I. Centralisation of the radial club hand by gradual distraction. J Hand Surg Br. 1989. 14(1):37–42.
Article15. Bora FW Jr, Osterman AL, Kaneda RR, Esterhai J. Radial club-hand deformity: long-term follow-up. J Bone Joint Surg Am. 1981. 63(5):741–745.
Article16. Buck-Gramcko D. Radialization as a new treatment for radial club hand. J Hand Surg Am. 1985. 10(6 Pt 2):964–968.
Article17. Smith AA, Greene TL. Preliminary soft tissue distraction in congenital forearm deficiency. J Hand Surg Am. 1995. 20(3):420–424.
Article18. Nanchahal J, Tonkin MA. Pre-operative distraction lengthening for radial longitudinal deficiency. J Hand Surg Br. 1996. 21(1):103–107.
Article19. Sabharwal S, Finuoli AL, Ghobadi F. Pre-centralization soft tissue distraction for Bayne type IV congenital radial deficiency in children. J Pediatr Orthop. 2005. 25(3):377–381.
Article20. Goldfarb CA, Murtha YM, Gordon JE, Manske PR. Soft-tissue distraction with a ring external fixator before centralization for radial longitudinal deficiency. J Hand Surg Am. 2006. 31(6):952–959.
Article21. Taghinia AH, Al-Sheikh AA, Upton J. Preoperative soft-tissue distraction for radial longitudinal deficiency: an analysis of indications and outcomes. Plast Reconstr Surg. 2007. 120(5):1305–1312.
Article22. Kanojia RK, Sharma N, Kapoor SK. Preliminary soft tissue distraction using external fixator in radial club hand. J Hand Surg Eur Vol. 2008. 33(5):622–627.
Article23. Lamb DW, Scott H, Lam WL, Gillespie WJ, Hooper G. Operative correction of radial club hand: a long-term follow-up of centralization of the hand on the ulna. J Hand Surg Br. 1997. 22(4):533–536.24. McCarthy JJ, Kozin SH, Tuohy C, Cheung E, Davidson RS, Noonan K. External fixation and centralization versus external fixation and ulnar osteotomy: the treatment of radial dysplasia using the resolved total angle of deformity. J Pediatr Orthop. 2009. 29(7):797–803.
Article25. Goldfarb CA, Klepps SJ, Dailey LA, Manske PR. Functional outcome after centralization for radius dysplasia. J Hand Surg Am. 2002. 27(1):118–124.
Article26. Heikel HV. Aplasia and hypoplasa of the radius: studies on 64 cases and on epiphyseal transplantation in rabbits with the imitated defect. Acta Orthop Scand Suppl. 1959. 39:1–155.27. Hurwitz PJ. Experimental transplantation of small joints by microvascular anastomoses. Plast Reconstr Surg. 1979. 64(2):221–231.
Article28. Zaleske DJ, Ehrlich MG, Piliero C, May JW Jr, Mankin HJ. Growth-plate behavior in whole joint replantation in the rabbit. J Bone Joint Surg Am. 1982. 64(2):249–258.
Article29. Brown K, Marie P, Lyszakowski T, Daniel R, Cruess R. Epiphysial growth after free fibular transfer with and without microvascular anastomosis: experimental study in the dog. J Bone Joint Surg Br. 1983. 65(4):493–501.
Article30. Vilkki SK. Advances in microsurgical reconstruction of the congenitally adactylous hand. Clin Orthop Relat Res. 1995. (314):45–58.
Article31. Mathes SJ, Buchannan R, Weeks PM. Microvascular joint transplantation with epiphyseal growth. J Hand Surg Am. 1980. 5(6):586–589.
Article32. Vilkki SK. Canadell J, Ferial F, Lazo-Zbikowski J, editors. Distraction lengthening and microvascular bone transplantation in the treatment of radial club hand. Proceedings of the 14th International Hoff man External Fixation Conference. 1992. Pampolona, Spain: EUROGRAF;249–251.33. Albee FH. Formation of radius congenitally absent: condition seven years after implantation of bone graft. Ann Surg. 1928. 87(1):105–110.34. Starr DE. Congenital absence of the radius: a method of surgical correction. J Bone Joint Surg Am. 1945. 27(4):572–577.35. Vilkki SK. Vascularized joint transfer for radial club hand. Tech Hand Up Extrem Surg. 1998. 2(2):126–137.
Article36. Vilkki SK. Distraction and microvascular epiphysis transfer for radial club hand. J Hand Surg Br. 1998. 23(4):445–452.
Article37. de Pablos J Jr, Canadell J. Experimental physeal distraction in immature sheep. Clin Orthop Relat Res. 1990. (250):73–80.
Article38. Catagni MA, Szabo RM, Cattaneo R. Preliminary experience with Ilizarov method in late reconstruction of radial hemimelia. J Hand Surg Am. 1993. 18(2):316–321.
Article39. Hadidi AT, Kaddah NT, Zaki MS, Sami A, Aal NA. Congenital malformations of the hand: a study of the vascular pattern. J Hand Surg Br. 1990. 15(2):171–180.
Article40. Damore E, Kozin SH, Thoder JJ, Porter S. The recurrence of deformity after surgical centralization for radial clubhand. J Hand Surg Am. 2000. 25(4):745–751.
Article