J Korean Med Sci.
2007 Aug;22(4):682-686. 10.3346/jkms.2007.22.4.682.
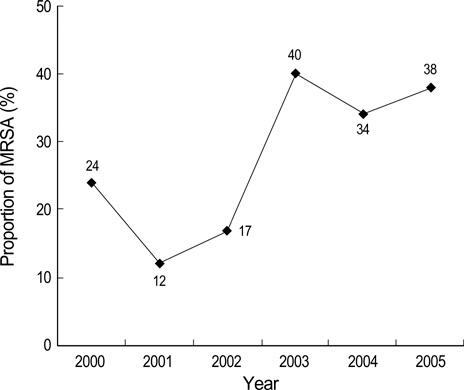
Analysis of Methicillin Resistance among Staphylococcus aureus Blood Isolates in an Emergency Department
- Affiliations
-
- 1Division of Infectious Diseases, Gyeongsang National University Hospital, Gyeongsang National University, Jinju, Korea.
- 2Division of Infectious Diseases, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. krpeck@smc.samsung.co.kr
- 3Department of Laboratory Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Division of Infectious Diseases, Dongsan Medical Center, Keimyung University, Daegu, Korea.
- 5Division of Infectious Diseases, Famtima Hospital, Daegu, Korea.
- 6Asian-Pacific Research Foundation for Infectious Diseases (ARFID), Seoul, Korea.
- KMID: 1127087
- DOI: http://doi.org/10.3346/jkms.2007.22.4.682
Abstract
- The increasing prevalence of methicillin-resistant Staphylococcus aureus (MRSA) has become of great concern in both hospital and community settings. To evaluate the prevalence and risk factors for methicillin resistance among Staphylococcus aureus, blood isolates in our Emergency Department (ED) were collected. All patients with S. aureus bacteremia (SAB) who presented to the ED from January 2000 to August 2005 were included, and a retrospective study was performed. A total of 231 patients with SAB were enrolled (median age, 59 yr; M:F, 125:106). Among these patients, methicillin-resistant strains accounted for 27.3% (63 patients). Catheter-related infection was the most frequent primary site of SAB (39.0%), followed by skin and soft tissue infection (16.5%). In multivariate analysis, recent surgery (OR, 3.41; 95% CI, 1.48-7.85), recent hospitalization (2.17; 1.06-4.62), and older age (> or =61 yr) (2.39; 1.25-4.57) were independently associated with the acquisition of methicillin-resistant strains. When antimicrobial therapy is considered for the treatment of a patient with suspected SAB, clinicians should consider obtaining cultures and modifying empirical therapy to provide MRSA coverage for patients with risk factors: older age, recent hospitalization, and recent surgery.
MeSH Terms
-
Adult
Age Factors
Aged
Anti-Bacterial Agents/pharmacology/therapeutic use
Cross Infection/blood/drug therapy/microbiology
Emergency Service, Hospital/statistics & numerical data
Female
Humans
Male
Methicillin/pharmacology/*therapeutic use
*Methicillin Resistance
Middle Aged
Multivariate Analysis
Retrospective Studies
Risk Factors
Staphylococcal Infections/blood/drug therapy/*microbiology
Staphylococcus aureus/*drug effects/isolation & purification
Figure
Reference
-
1. Naimi TS, LeDell KH, Como-Sabetti K, Borchardt SM, Boxrud DJ, Etienne J, Johnson SK, Vandenesch F, Fridkin S, O'Boyle C, Danila RN, Lynfield R. Comparison of community- and health care-associated methicillin-resistant Staphylococcus aureus infection. JAMA. 2003. 290:2976–2984.2. Sattler CA, Mason EO Jr, Kaplan SL. Prospective comparison of risk factors and demographic and clinical characteristics of community-acquired, methicillin-resistant versus methicillin-susceptible Staphylococcus aureus infection in children. Pediatr Infect Dis J. 2002. 21:910–917.
Article3. Fridkin SK, Hageman JC, Morrison M, Sanza LT, Como-Sabetti K, Jernigan JA, Harriman K, Harrison LH, Lynfield R, Farley MM. Methicillin-resistant Staphylococcus aureus disease in three communities. N Engl J Med. 2005. 352:1436–1444.4. Salgado CD, Farr BM, Calfee DP. Community-acquired methicillin-resistant Staphylococcus aureus: a meta-analysis of prevalence and risk factors. Clin Infect Dis. 2003. 36:131–139.5. Frazee BW, Lynn J, Charlebois ED, Lambert L, Lowery D, Perdreau-Remington F. High prevalence of methicillin-resistant Staphylococcus aureus in emergency department skin and soft tissue infections. Ann Emerg Med. 2005. 45:311–320.
Article6. Kim SH, Park WB, Lee KD, Kang CI, Choe YJ, Kim HB, Park SW, Kim US, Oh MD, Kim EC, Choe KW. The effects of initial empirical antibiotics regimens on the outcomes of Staphylococcus aureus bacteremia. Korean J Infect Dis. 2002. 34:293–304.7. Kim HB, Kim T, Lee BB, Kim US, Park SW, Shin JW, Oh MD, Kim EC, Lee YS, Kim BS, Choe KW. Frequency of resistance to aminog lycoside antibiotics in staphy lococcus aureus isolated from tertiary hospitals. Korean J Infect Dis. 2002. 34:39–46.8. Kim YJ. A study of prevalence and antibiotic susceptibilities of staphylococcus aureus in the bacterial skin infection of dermatology outpatients. Korean J Dermatol. 2001. 39:866–871.9. Kim HB, Sa CM, Yoo J, Kim BS, Yun OJ, Yoon HR, Lee YS. Antibiotic resistance patterns of Staphylococcus aureus isolated from the patients admitted to non-tertiary hospitals. Korean J Infect Dis. 2000. 32:259–263.10. Kim US, Bang JH, Kim HB, Park SW, Oh MD, Song YW, Kim CH, Kim EC, Choe KW. Epidemiology of and risk factors for methicillin resistance in community-acquired and nosocomial Staphylococcus aureus bacteremia. Korean J Infect Dis. 1999. 31:325–331.11. Moran GJ, Krishnadasan A, Gorwitz RJ, Fosheim GE, McDougal LK, Carey RB, Talan DA. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006. 355:666–674.12. Lodise TP, McKinnon PS, Swiderski L, Rybak MJ. Outcomes analysis of delayed antibiotic treatment for hospital-acquired Staphylococcus aureus bacteremia. Clin Infect Dis. 2003. 36:1418–1423.
Article13. Rezende NA, Blumberg HM, Metzger BS, Larsen NM, Ray SM, McGowan JE Jr. Risk factors for methicillin-resistance among patients with Staphylococcus aureus bacteremia at the time of hospital admission. Am J Med Sci. 2002. 323:117–123.
Article14. Standards NCCLS. Performance Standards for Antimicrobial Disk Susceptibility Tests-Eight Deition: Approved Standard M100-S13 (M2). 2003. Wayne, PA, USA: NCCLS.15. Mermel LA, Farr BM, Sherertz RJ, Raad II, O'Grady N, Harris JS, Craven DE. Guidelines for the management of intravascular catheter-related infections. Clin Infect Dis. 2001. 32:1249–1272.
Article16. Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med. 1994. 96:200–209.17. Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections. Am J Infect Control. 1988. 16:128–140.18. Chambers HF. The changing epidemiology of Staphylococcus aureus? Emerg Infect Dis. 2001. 7:178–182.
Article19. Kim SH, Park WB, Lee KD, Kang CI, Bang JW, Kim HB, Kim EC, Oh MD, Choe KW. Outcome of inappropriate initial antimicrobial treatment in patients with methicillin-resistant Staphylococcus aureus bacteraemia. J Antimicrob Chemother. 2004. 54:489–497.
Article20. Jernigan JA, Pullen AL, Partin C, Jarvis WR. Prevalence of and risk factors for colonization with methicillin-resistant Staphylococcus aureus in an outpatient clinic population. Infect Control Hosp Epidemiol. 2003. 24:445–450.21. Charlebois ED, Bangsberg DR, Moss NJ, Moore MR, Moss AR, Chambers HF, Perdreau-Remington F. Population-based community prevalence of methicillin-resistant Staphylococcus aureus in the urban poor of San Francisco. Clin Infect Dis. 2002. 34:425–433.
Article22. Goetz A, Posey K, Fleming J, Jacobs S, Boody L, Wagener MM, Muder RR. Methicillin-resistant Staphylococcus aureus in the community: a hospital-based study. Infect Control Hosp Epidemiol. 1999. 20:689–691.23. Cosgrove SE, Sakoulas G, Perencevich EN, Schwaber MJ, Karchmer AW, Carmeli Y. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis. 2003. 36:53–59.24. Blot SI, Vandewoude KH, Hoste EA, Colardyn FA. Outcome and attributable mortality in critically Ill patients with bacteremia involving methicillin-susceptible and methicillin-resistant Staphylococcus aureus. Arch Intern Med. 2002. 162:2229–2235.
Article25. Wyllie DH, Peto TE, Crook D. MRSA bacteraemia in patients on arrival in hospital: a cohort study in Oxfordshire 1997-2003. BMJ. 2005. 331:992.
Article26. Huang SS, Platt R. Risk of methicillin-resistant Staphylococcus aureus infection after previous infection or colonization. Clin Infect Dis. 2003. 36:281–285.27. Harbarth S, Rutschmann O, Sudre P, Pittet D. Impact of methicillin resistance on the outcome of patients with bacteremia caused by Staphylococcus aureus. Arch Intern Med. 1998. 158:182–189.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A statistical analysis of methicillin-resistant staphylococcus aureus
- Detection of Multidrug Resistant Patterns and Associated - genes of Methicillin Resistant Staphylococcus aureus ( MRSA ) Isolated from Clinical Specimens
- Characteristics of methicillin-resistant staphylococcus aureus isolates from various clinical materials
- Detection of Methicillin Resistance in Staphylococcus aureus by 2% NaCl Mueller-Hinton Agar and Mannitol Salt Agar
- A Survey for Methicillin - Resistant Staphylococcus Aureus