Korean J Radiol.
2008 Dec;9(6):541-549. 10.3348/kjr.2008.9.6.541.
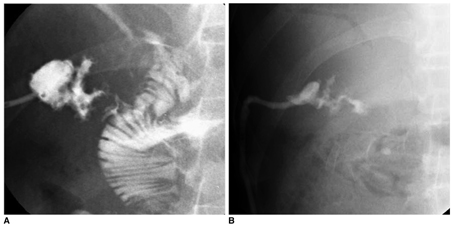
Interventional Management of Gastrointestinal Fistulas
- Affiliations
-
- 1Department of Diagnostic Radiology, Kyung Hee University Medical Center, Seoul, Korea. ohjh6108@hanmail.net
- 2Department of Surgery, Kyung Hee University Medical Center, Seoul, Korea.
- KMID: 1118876
- DOI: http://doi.org/10.3348/kjr.2008.9.6.541
Abstract
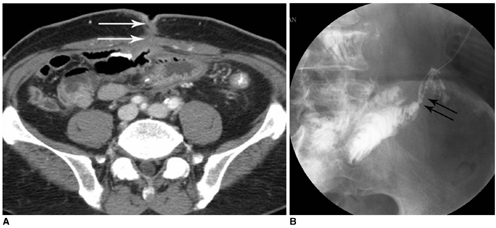
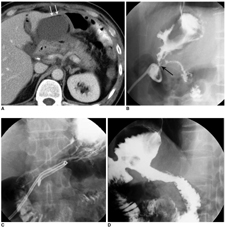
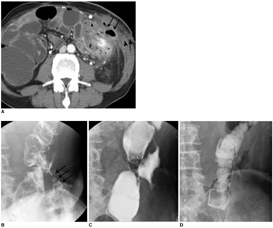
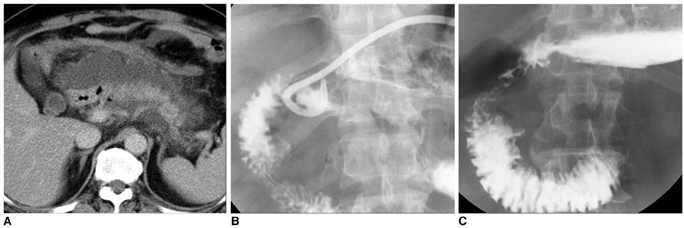
- Gastrointestinal (GI) fistulas are frequently very serious complications that are associated with high morbidity and mortality. GI fistulas can cause a wide array of pathophysiological effects by allowing abnormal diversion of the GI contents, including digestive fluid, water, electrolytes, and nutrients, from either one intestine to another or from the intestine to the skin. As an alternative to surgery, recent technical advances in interventional radiology and percutaneous techniques have been shown as advantageous to lower the morbidity and mortality rate, and allow for superior accessibility to the fistulous tracts via the use of fistulography. In addition, new interventional management techniques continue to emerge. We describe the clinical and imaging features of GI fistulas and outline the interventional management of GI fistulas.
Keyword
MeSH Terms
Figure
Reference
-
1. Falconi M, Pederzoli P. The relevance of gastrointestinal fistulae in clinical practice: a review. Gut. 2001. 49:Suppl 4. iv2–iv10.2. Gonzalez-Pinto I, Gonzalez EM. Optimising the treatment of upper gastrointestinal fistulae. Gut. 2001. 49:Suppl 4. iv22–iv31.3. McLean GK, Mackie JA, Freiman DB, Ring EJ. Enterocutaneous fistulae: interventional radiologic management. AJR Am J Roentgenol. 1982. 138:615–619.4. Boverie JH, Remont A. Dondelinger RF, Rossi P, Kurdziel JC, Wallace S, editors. Percutaneous management of fistulas in the digestive tract. Interventional radiology. 1990. Stuttgart: Thieme;746–753.5. Berry SM, Fischer JE. Classification and pathophysiology of enterocutaneous fistulas. Surg Clin North Am. 1996. 76:1009–1018.6. LaBerge JM, Kerlan RK Jr, Gordon RL, Ring EJ. Nonoperative treatment of enteric fistulas: results in 53 patients. J Vasc Interv Radiol. 1992. 3:353–357.7. Han JK. Han MC, Park JH, editors. Percutaneous abdominal abscess drainage. Interventional radiology. 1999. Seoul: Ilchokak;707–714.8. Grunshaw ND, Ball CS. Palliative treatment of an enterorectal fistula with a covered metallic stent. Cardiovasc Intervent Radiol. 2001. 24:438–440.9. Kang YJ, Oh JH, Yoon Y, Kim EJ, Ryu KN, Lim JW, et al. Covered metallic stent placement in the treatment of postoperative fistula resistant to conservative management after Billroth I operation. Cardiovasc Intervent Radiol. 2005. 28:90–92.10. Rabago LR, Ventosa N, Castro JL, Marco J, Herrera N, Gea F. Endoscopic treatment of postoperative fistulas resistant to conservative management using biological fibrin glue. Endoscopy. 2002. 34:632–638.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of interventional radiology in the management of postoperative gastrointestinal leakage
- Interventional radiological approaches to non-variceal gastrointestinal bleeding
- Complications of Arteriovenous Hemodialysis Fistulas: Anglographic Findings and Interventional Treatments
- Over-the-Scope Clip in the Treatment of Gastrointestinal Leaks and Perforations
- The use of OverStitchâ„¢ for the treatment of intestinal perforation, fistulas and leaks